RWCS 2016 – OA/OP, Gout, Sarcoid & JIA Reviewed Save
Recent Developments in Osteoarthritis, Osteoporosis and Gout
Drs. Orin Troum and Martin Bergman reviewed the literature and news from 2015 for advances in OA, OP and gout. Hydroxychloroquine has been shown to have no effect in hand OA based on a RCT in 196 patients - no significant change in pain or function (this has also been shown for inflammatory OA in the past).
Intraarticular (IA) corticosteroids – while these may be safe when used sparingly, a recent study of frequent steroid IA injections failed to demonstrate any benefits. A two-year randomized, controlled clinical trial (RCT) show that when IA triamcinolone hexacetonide (40 mg vs saline) was given every 12 weeks over two years to symptomatic OA (with ultrasound evidence of synovitis), no significant differences in WOMAC pain, walk time, or structural endpoints. A low rate 3% of HTN and hyperglycemia was seen.
In July 2015, the FDA strengthened its warnings regarding NSAID use and risk of MI and CVA. Risk may increase early (within weeks) and goes up with prolonged use or higher doses, especially in those with preexisting heart disease. Those who take NSAIDs after their first MI have a higher risk of death in the following year.
An October 22, 2015 NEJM report showed knee replacement surgery was superior to nonsurgical knee management (in OA) when looking at 12-month pain, ADL and quality of life outcomes.
Following total joint replacement, there is an increased risk of MI; up to nine-fold higher in the first month post-op (AR 67:2771, 2015).
The big news in gout this year was the new approval of lesinurad (Zurampic) - approved in late 2015 as adjunctive therapy along with other urate-lowering therapy (ULT). The pivotal data came from the CLEAR 1 (n=603), CRYSTAL (324) and LIGHT (214) clinical trials. The drug should not be used as monotherapy. The approved dose of lesinurad is 200 mg qd. Creatinine doubles in 2-8% of patients in a dose-dependent manner, hence there is a black box warning for renal failure. Much of the discussion on this was how potent was this combination of lesinurad plus ULT (allopurinol or febuxostat) compared with optimizing or maximizing allopurinol use. Data clearly shows all doctors, including rheumatologists, seldom use allopurinol doses > 300 mg/day.
Chronic colchicine use may be associated with a 49% reduction in cardiovascular events and a 73% reduction in all-cause mortality.
Numerous gout reports showed comorbidities and associations including dementia, sleep apnea, septic arthritis, erectile dysfunction and a seasonal variation with peak incidence in autumn and lower rates in the spring.
Sarcoidosis Update
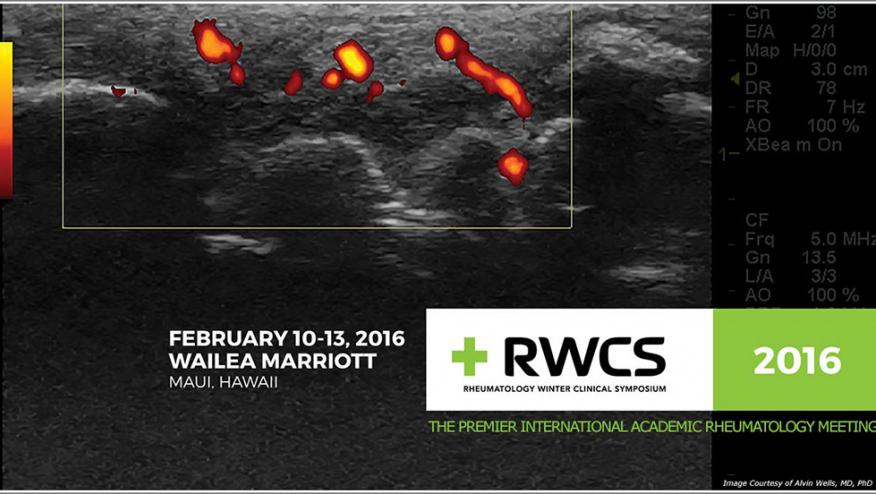
Dr. Alvin Wells discussed sarcoid and offered up some pearls for consideration. In the 1970s, the question centered around whether sarcoidosis may be due to an infection.
Pearl #1: consider infection if you’re considering a diagnosis of sarcoidosis – he recommends ordering IGRA, ASO, and urine C&S
After reviewing the role of Th17 and TREG cells in the pathogenesis, he focused on clinical manifestations. At presentation, most patients present for respiratory and constitutional complaints, often with adenopathy. For many the lung dominates the clinical picture. Interestingly, autopsy series show more subclinical muscle and liver infiltration by sarcoid granulomas. Skin features include lupus pernio, but noted that keloids or nodular changes in tattoos should lead one to consider sarcoid. Osteoarticular manifestations from one series included arthralgias, inflammatory arthritis in 51%, Lofgrens syndrome in 7%, chronic polyarthritis in 32%, oligoarthritis in 8% and dactylitis in 14%. Ocular involvement with uveitis is also common. Pain may be from osteoarticular disease or neuropathy.
Pearl #2 - When pain is not explained, consider small fiber neuropathy
Serum angiotensin converting enzyme levels (ACE) does not correlate well with disease activity.
Treatment of sarcoid has a variety of agents, with no one agent being dominant. Corticosteroids are the mainstay, given as 1 mg/kg for ocular and pulmonary disease. Be sure to treat for glucocorticoid-induced osteoporosis and consider prophylaxis for pneumocystis infection. DMARDS have been tried as steroid-sparing agents including MTX, leflunomide, azathioprine, and mycophenolate. Hydroxychloroquine can be used to treat the skin disease and hypercalcemia. Cytotoxics (CTX or chlorambucil) are rarely used for aggressive eye disease. Lastly, pentoxyphylline and thalidomide have been used in resistant cases of lupus pernio.
Pediatric Rheumatology for the Adult Rheumatologists
Dr. Anne Stevens began by reviewing the diagnostic approach. When faced with a juvenile with few swollen joints the differential diagnosis includes juvenile idiopathic arthritis (JIA), reactive arthritis (due to Strept?), septic arthritis, osteomyelitis, or toxic synovitis of the hip. Post-streptococcal reactive arthritis is unique by having positive Strept serologies, normal ECHO, and a poor response to NSAIDs. The current treatment is Bicillin every three weeks for one year (follow ECHO annually).
She presented another case of a 14 year old boy with knee pain, swelling for 8 weeks and an elevated LDH-4500. Is this JIA or malignancy? Potential cancers in this situation include leukemia, lymphoma, osteosarcoma and neuroblastoma. Clues for malignancy include too much pain, looking sicker, fever, night sweats, weight loss, organomegaly, bone pain and back pain – kids don’t get back pain!
Raynaud's in children should raise suspicion. This does not include children with acrocyanosis or those taking methylphenidate (or like Rx) for ADD who are prone to red fingers. 30% of kids with true Raynaud's will develop a connective tissue disease within six years (mean two years). It is important to look at capillaroscopy, but only 1/3 have typical sclerodermatous capillary changes. However, there is no risk of CTD if the capillaroscopy is normal and the ANA is negative.
Chronic anterior uveitis commonly accompanies oligoarticular JIA (formerly pauciarticular JRA). This subset requires > 6 weeks of fewer than 5 joints, usually hips and knees, 20% may have asymptomatic anterior uveitis and ANA+ - they are never RF or CCP+. Such kids need slit lamp exam every three months, largely because this is the leading cause of childhood blindness. Complications include band keratopathy, maculopathy, and glaucomatous optic neuropathy. Treat the inflammatory eye disease with topical steroids, MTX, cyclosporine, azathioprine, mycophenolate, infliximab, adalimumab or rituximab. They often require higher doses.
TMJ arthritis may occur in 29-71 % of all JIA patients. Unfortunate outcomes include micrognathia, and dental problems.
Treatment and outcomes were reviewed. Notably the adult measure ACR20/50/70, does not perform well in JIA. Instead they use definitions like Clinically inactive disease (CID) which is replacing the JCR30 or Pediatric ACR20/50/70. New paradigm for JIA – treat early and treat aggressively to remission.
The majority of JIA kids will have active arthritis into adulthood. While 44 % achieve remission, but few (<10%) are off meds at five years.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.