EULAR Recommendations on Large Vessel Vasculitis Save
Th European League Against Rheumatism (EULAR) recommendations for the management of large vessel vasculitis (LVV) was originally published in 2009. Since then there have been new randomised clinical trials and cohort analyses leading to an update the original recommendations.
A EULAR international task force undertook a systematic literature review and sought input from 20 experts from 13 countries, including rheumatologists, internists, immunologists, a neurologist, a neuro-ophthalmologist and an epidemiologist, one health professional and two patients affected by LVV.
This guidance has 3 overarching principles, and 10 recommendations were put forth.
We recommend that the diagnosis of LVV should be confirmed by imaging or histology.
High dose glucocorticoid therapy (40–60 mg/day prednisone-equivalent) should be initiated immediately for induction of remission in active giant cell arteritis (GCA) or Takayasu arteritis (TAK).
We recommend adjunctive therapy in selected patients with GCA using tocilizumab, with methotrexate as an alternative. Non-biological glucocorticoid-sparing agents should be given in combination with glucocorticoids in all patients with TAK and biological agents may be used in refractory or relapsing patients. We no longer recommend the routine use of antiplatelet or anticoagulant therapy for treatment of LVV unless it is indicated for other reasons.
Overarching Principles
- Patients with LVV should be offered best care which must be based on a shared decision between the patient and the rheumatologist, considering efficacy, safety and costs
- Patients should have access to education focusing on the impact of LVV, key warning symptoms and its treatment and complications
- Patients with LVV should be screened for treatment-related and cardiovascular comorbidities, with an attention to prophylaxis and life-style advice to reduce cardiovascular risk and treatment-related complications
Recommendations
- Patients presenting with signs and symptoms suggestive of GCA should be urgently referred to a specialist team for further multidisciplinary diagnostic work-up and management.
- Patients presenting with signs and symptoms suggestive of TAK should be referred to a specialist team for multidisciplinary diagnostic work-up and management.
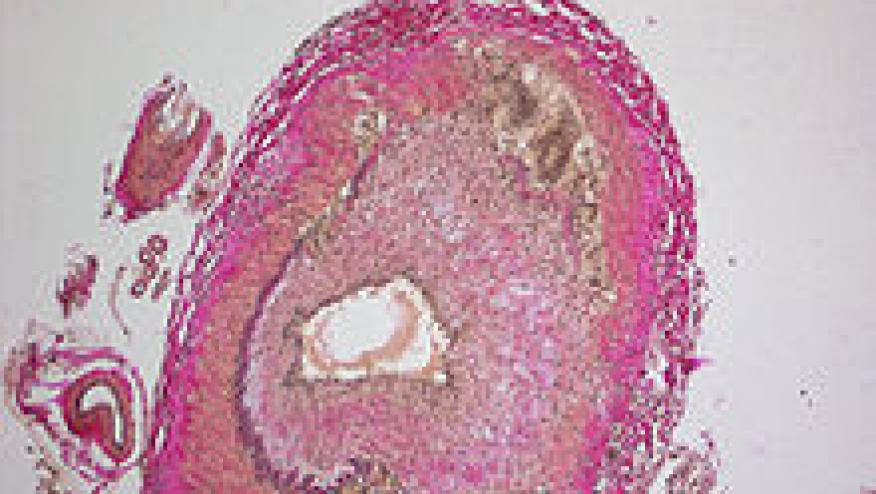
- A suspected diagnosis of LVV should be confirmed by imaging (ultrasound or MRI for temporal or other cranial arteries, ultrasound, CT, PET-CT or MRI for the aorta/extracranial arteries or histology (Temporal artery biopsy)
- High dose glucocorticoid (GC) therapy (40–60 mg/day prednisone-equivalent) should be initiated immediately for induction of remission in active GCA or TAK.
- Once disease is controlled, we recommend tapering the GC dose to a target dose of 15–20 mg/day within 2–3 months and after 1 year to ≤5 mg/day (for GCA) and to ≤10 mg/day (for TAK).
- Adjunctive therapy should be used in selected patients with GCA (refractory or relapsing disease, the presence or an increased risk of GC related adverse effects or complications) using tocilizumab, or alternatively, methotrexate
- Non-biologic disease modifying agents should be given in combination with GC in all patients with TAK. Tocilizumab or TNF-inhibitors can be considered in case of relapsing or refractory disease despite conventional DMARD therapy.
- In case of major relapse (either with signs or symptoms of ischaemia or progressive vascular inflammation) we recommend reinstitution or dose escalation of GC therapy as recommended for new onset disease.## For minor relapses we recommend an increase in GC dose at least to the last effective dose.* Initiation or modification of adjunctive therapy should be considered particularly after recurrent disease relapses.
- Antiplatelet or anticoagulant therapy should not be routinely used for treatment of LVV unless it is indicated for other reasons (eg, coronary heart disease or cerebrovascular disease etc). In LVV, elective endovascular interventions or reconstructive surgery should be performed in phases of stable remission. However, arterial vessel dissection or critical vascular ischaemia requires urgent referral to a vascular team.
- Regular follow-up and monitoring of disease activity in patients with LVV is recommended, primarily based on symptoms, clinical findings and ESR/CRP levels.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.