New EULAR/ACR Classification Criteria for Adult and Juvenile Myositis Save
The European League Against Rheumatism and the American College of Rheumatology (EULAR/ACR) have developed classification criteria for idiopathic inflammatory myopathies (IIM) based on data from 976 IIM patients (74% adults; 26% children) and 624 non-IIM patients with mimicking conditions (82% adults; 18% children) from 47 rheumatology, dermatology, neurology and paediatric clinics worldwide.
The new criteria allow classification of ‘definite’, ‘probable’ and ‘possible’ IIM, in addition to the major subgroups of IIM, including juvenile IIM and have been shown to perform better than existing criteria.
Recommendations
- Patients with pathognomonic skin rashes (heliotrope rash, Gottron’s papules and/or Gottron’s sign) of JDM or DM are accurately classified with the EULAR/ACR classification criteria without including muscle biopsy data. For patients without these skin manifestations, muscle biopsy is recommended. For DM patients without muscle involvement, a skin biopsy is recommended.
- The minimum required to classify as "probable IIM" would be a score of 5.5 (6.7 with muscle biopsy) which had good sensitivity/specificity (87%/82% without biopsies, 93%/88% with biopsies)
- "Definite IIM" (with a probability of ≥90%) was achieved with a score of ≥7.5 (≥8.7 with muscle biopsy),
- Having a score of <5.3 (<6.5 with muscle biopsy), rules out IIM as a possibility.
The criteria were developed based on statistical models, 16 variables that best distinguished IIM cases from comparators were chosen and each variable was assigned a weighted score (with or without biospy evidence).
| When no better explanation for the symptoms and signs exists, these classification criteria can be used | |||
| Variable | Score points | Definition | |
| Without muscle biopsy | With muscle biopsy | ||
| Age of onset | |||
| Age of onset of first symptom assumed to be related to the disease ≥18 years and <40 years | 1.3 | 1.5 | 18≤Age (years) at onset of first symptom assumed to be related to the disease <40 |
| Age of onset of first symptom assumed to be related to the disease ≥40 years | 2.1 | 2.2 | Age (years) at onset of first symptom assumed to be related to the disease ≥40 |
| Muscle weakness | |||
| Objective symmetric weakness, usually progressive, of the proximal upper extremities | 0.7 | 0.7 | Weakness of proximal upper extremities as defined by manual muscle testing or other objective strength testing, which is present on both sides and is usually progressive over time |
| Objective symmetric weakness, usually progressive, of the proximal lower extremities | 0.8 | 0.5 | Weakness of proximal lower extremities as defined by manual muscle testing or other objective strength testing, which is present on both sides and is usually progressive over time |
| Neck flexors are relatively weaker than neck extensors | 1.9 | 1.6 | Muscle grades for neck flexors are relatively lower than neck extensors as defined by manual muscle testing or other objective strength testing |
| In the legs, proximal muscles are relatively weaker than distal muscles | 0.9 | 1.2 | Muscle grades for proximal muscles in the legs are relatively lower than distal muscles in the legs as defined by manual muscle testing or other objective strength testing |
| Skin manifestations | |||
| Heliotrope rash | 3.1 | 3.2 | Purple, lilac-coloured or erythematous patches over the eyelids or in a periorbital distribution, often associated with periorbital oedema |
| Gottron’s papules | 2.1 | 2.7 | Erythematous to violaceous papules over the extensor surfaces of joints, which are sometimes scaly. May occur over the finger joints, elbows, knees, malleoli and toes |
| Gottron’s sign | 3.3 | 3.7 | Erythematous to violaceous macules over the extensor surfaces of joints, which are not palpable |
| Other clinical manifestations | |||
| Dysphagia or oesophageal dysmotility | 0.7 | 0.6 | Difficulty in swallowing or objective evidence of abnormal motility of the oesophagus |
| Laboratory measurements | |||
| Anti-Jo-1 (anti-histidyl-tRNA synthetase) autoantibody present | 3.9 | 3.8 | Autoantibody testing in serum performed with standardised and validated test, showing positive result |
| Elevated serum levels of creatine kinase (CK)* or lactate dehydrogenase (LD)* or aspartate aminotransferase (ASAT/AST/SGOT)* or alanine aminotransferase (ALAT/ALT/SGPT)* |
1.3 | 1.4 | The most abnormal test values during the disease course (highest absolute level of enzyme) above the relevant upper limit of normal |
| Muscle biopsy features—presence of: | |||
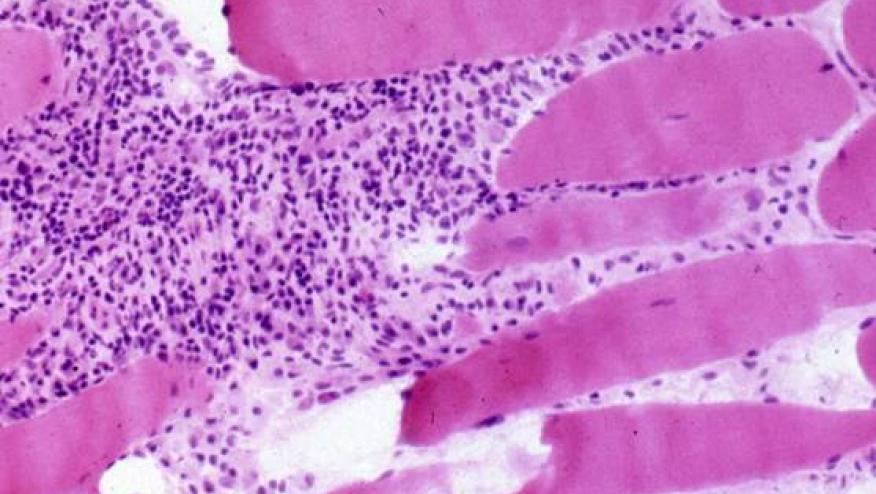
| Endomysial infiltration of mononuclear cells surrounding, but not invading, myofibres | 1.7 | Muscle biopsy reveals endomysial mononuclear cells abutting the sarcolemma of otherwise healthy, non-necrotic muscle fibres, but there is no clear invasion of the muscle fibres | |
| Perimysial and/or perivascular infiltration of mononuclear cells | 1.2 | Mononuclear cells are located in the perimysium and/or located around blood vessels (in either perimysial or endomysial vessels) | |
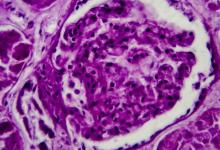
| Perifascicular atrophy | 1.9 | Muscle biopsy reveals several rows of muscle fibres, which are smaller in the perifascicular region than fibres more centrally located | |
| Rimmed vacuoles | 3.1 | Rimmed vacuoles are bluish by H&E staining and reddish by modified Gomori trichrome stains | |
-
*Serum levels above the upper limit of normal.
EULAR/ACR classification criteria for adult and juvenile idiopathic inflammatory myopathies (IIMs)










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.