Venous Thromboembolism Increased with Rheumatoid Arthritis, Not with TNF Inhibition Save
Venous thromboembolism (VTE) is a common adverse event throughout medicine and includes both pulmonary embolism (PE) and deep vein thrombosis (DVT). The cost of diagnosing a thromboembolic event is approximately $4000 - $5550, while the annual cost of treating one case of VTE is between $17,000 and $19,000. The impact of VTE is substantial.
More deaths result from VTE than from myocardial infarctions mainly due to the difficulty of diagnosis and prevention. VTE risk increases with suggestive signs and symptoms (Wells’ criteria), and evidence for VTE can be confirmed by D-dimer levels, extremity compression ultrasound, ventilation-perfusion scan, or pulmonary CT angiography.
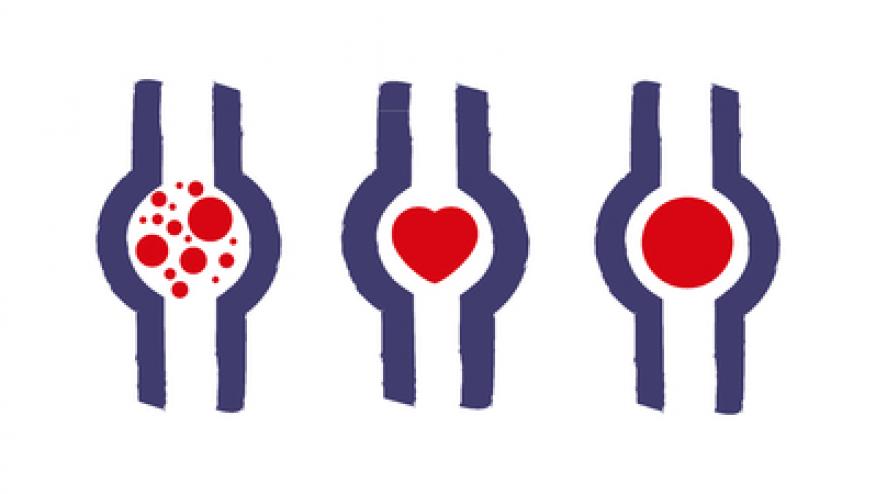
A total of one million cases of new and recurrent venous thromboembolism occur yearly in the United States, with two-thirds developing in hospitalized patients. PE accounts for 5 to 10% of deaths in hospitalized patients; yet, VTE is the most common preventable cause of in-hospital death. Risk factors for VTE include immobility, age and obesity. VTE risks can be explained by the pathophysiology considered in Virchow’s triad: injury to vascular endothelium, stasis of flow, and activation of the coagulation cascade.
Certain factors can increase the development of all three elements of Virchow’s triad, including fracture, hip or knee replacement, trauma, surgery, cancer, chemotherapy, heart failure, oral contraceptive treatment, pregnancy, or prior history of VTE. There are also genetic risk factors that increase the risk of VTE, including deficiencies of protein C and S, antithrombin, factor V Leiden mutation and increased homocysteine or factor VIII. The lupus anticoagulant and anti-cardiolipin autoimmune markers have also been associated with an increased risk of VTE. The role of inflammation as a risk factor for VTE has only recently been defined.
VTE and Inflammatory Disorders. Autoimmune disorders, including rheumatoid arthritis (RA), SLE, antiphospholipid syndrome, Wegener’s granulomatosis, and inflammatory bowel disease, have been associated with an increased risk of thromboembolic events. Many factors have linked inflammation and autoimmunity with hypercoagulability leading to thromboembolism
Inflammation increases cytokine production and inhibits protein C, leading to increased coagulability. In a large cohort study of 22,143 RA and 88,572 non-RA patients, the incidence ratio for VTE in RA was 6.1 per 1000 person years, 2.4 times higher (95%CI 2.1-2.8) than in non-RA patients.
Other studies similarly confirmed that the presence rheumatoid arthritis and other autoimmune diseases is an independent risk factor for PE and VTE; the risk is even higher in those who are hospitalized 10-12. One study suggested this association is due to RA patients having higher than normal fibrinogen levels, free factor VIII, free tissue factor pathway inhibitor (TFPI), and higher rates of thrombin formation. Although the increase in TFPI delays the clotting cascade, the increase in factor VIII results in faster thrombin formation, generating greater thrombus formation.
All of these elevated coagulation elements correlated with increased disease activity states. It is evident that controlling the disease, and reducing inflammation is a key factor to decreasing VTE risk. In a Swedish population study, VTE risk was not seen at the onset of RA, but was increased 2 fold in the first year and remained stable over the next 10 years. While VTE following hospitalization increased in RA, this was not higher than the comparison cohort after hospital discharge. VTE risk increased with age, but was not affected by sex or RF status.
Is the Incidence of VTE Higher with TNF Inhibitors? While it appears that inflammation and RA are associated with increased VTE events, there exists the possibility that the abrogation of inflammation by TNF inhibitors may lessen such risks15 In murine models, TNF has been associated with increased thrombus formation. Conversely, diminished thrombosis is seen in TNF receptor knockout mice or treatment with TNFα blockade.
Petitpain et al. found 85 thrombotic events seen in RA and IBD patients receiving TNFi in France from 2000-2006 ; these events were evenly categorized into arterial and venous thromboses). The presence of >2 risk factors for thromboses was more prevalent with arterial (16 of 42 patients) than with venous (4 of 43) thromboses. The authors suggested that TNFi may be associated with VTE, since events occurred in patients with no or few risk factors for venous thrombosis. In contrast,
The British Society for Rheumatology analyzed VTE rate in 15 554 RA patients (11 881 on anti-TNF, 3673 on DMARD) and found no increase in VTE risk for those receiving TNFi when compared with DMARD use (hazard ratio 0.8, 95%CI, 0.5 to 1.5) after adjusting for age, gender, baseline steroid exposure, smoking, disease duration, disease severity, and other comorbid conditions. Interestingly, Dutch investigators examined 272 RA patients treated with adalimumab (ADA) and found 8 VTE (2.9%), 4 of whom had anti-ADA antibodies (Abs). Since only 28% of this cohort had anti-ADA Abs, the incidence rate for VTE was 3 fold higher in patients with anti-ADA Abs, with an adjusted HR of 7.6 (95% CI 1.3-45.1) favoring VTE in patients with anti-ADA Abs (P = 0.025). The data suggest that anti-ADA Abs may interfere with drug effect, thereby enhancing the VTE risk annulled by TNF inhibition.
Summary. Whereas there is a clear mechanism for the increase in VTE events in RA and other autoimmune diseases, the same does not stand for those patients taking TNF inhibitors. RA leads to amplified inflammation, indirectly increasing the rate of venous thromboembolism. TNF inhibitors have recently been studied and shown to offset the thrombotic propensity seen with active rheumatoid inflammation.
Authored by Anusha Ganesh, John J. Cush, Kathryn H. Dao. This overview originally appeared in the ACR Drug Safety Quarterly November 2012.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.