Best Imaging Techniques for non ANCA Vasculitis Save
Large vessel vasculitis (LVV) and CNS vasculitis are rare subsets of vasculitis. The challenges related to these diseases are well known to the rheumatologists who treat around the world. There are many articles stating that a delay in diagnosis of these diseases leads to increased morbidity and mortality. There are various imaging modalities, CT, MRI, PET, US- But which is the correct imaging to use and how to train the radiologists to identify using the correct feature for diagnosis and flare are reviewed and discussed at this meeting. At this time, particularly in terms of COVID-19, how can we diagnose and assess our patients in the least invasive way? This year there are a number of abstracts which discuss various ways to image.
As imaging has also improved over the years, this is the perfect opportunity to define how we image these difficult and rare diseases.
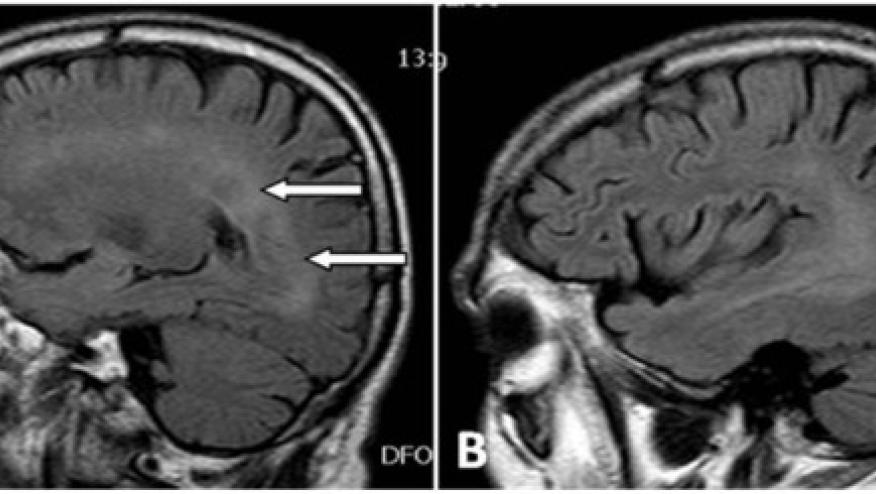
CNS vasculitis has many mimics that Dr. Hajj-Ali has worked on for years. There are useful clinical criteria but as we have increased our imaging capacities including improved MRI capabilities, there are now more unique and more precise techniques to assess the vessel wall. Imaging vessel walls through MRI or PET-CT can assess edema, thickness, enhancement, lesions, etc. Dr. Hajj-Ali has 2 posters looking at MRI in CNS vasculitis and wall enhancement (abstracts #0411, #0409). These considerations now need to be assessed in large prospective randomized trials
Another example of progress presented is about LVV and Takaysu’s arteritis. Dr. Kaitlin Quinn as the Vasculitis Research Consortium fellow has started to define those imaging modalities with the help of both Peter Grayson et al along with Dr. Peter Merkel and his team. These teams are also working within OMERACT to develop imaging outcome domains for use in clinical trials for these diseases. Takaysu’s arteritis is particularly challenging because we often find damage. We aggressively use immunosuppression due to the fear of damage, but we cannot adequately tell when patients flare.
In one poster, Dr. Quinn discusses the use of PET imaging which would improve diagnosis of Takayasu flares - Takaysu FD-PET-CT could aid in the diagnosis of flare ( abstracts #0428, #1928)
Further studies with imaging are needed to define interrater variability and there needs to be improved accessibility to these modalities. These modalities will hopefully be used in the United States and around the world to help with the diagnosis and management of these patients with difficult rare vasculitis diagnoses.
Join The Discussion
Still difficult if not impossible to diagnose CNS vasculitis by just imaging. Notoriously, neuro-radiologists tend to over-read these images, including the mentioning of "vasculitis" in just about every differential diagnosis, prompting rheumatology consults in a variety of different setting and diseases. That's the problem, since such a diagnosis would mandate immunosuppression. I have discontinued said therapy in many patients with diabetes and widespread atherosclerotic disease, diagnosed as having "CNS vasculitis". They all had a vasculopathy allright but not true vasculitis,










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.