BSR Guideline on Management of Sjögren disease Save

The British Society for Rheumatology has published its guideline for the management of adult and juvenile onset Sjogren's disease.
This guideline is an update to the 2017 guideline and is based on medical literature review focused on 19 clinical questions. While most of the diagnostic recommendations were "Strong", treatment recommendations were a mix of strong and "conditional" recommendation.
This guideline builds on and widens the recommendations published in 2017 and includes advice on the management of children and adolescents.
Select Recommendations based on Key Questions
What is the diagnostic accuracy of serologic testing in people suspected of SD?
- Do not measure ANA in the absence of clinical indicators of SD or other CTD
- Use ANA as a screening antibody where there is a clinical suspicion of CTD
- Measure ENA, even if the ANA is negative, if there is a high index of suspicion of SD
What is the diagnostic accuracy of salivary gland US scanning in people suspected of having SD?
- USS of the salivary glands can provide useful additional information to support either the presence of or lack of evidence for SD
- USS does not currently replace either antibody testing or histological analysis in adult SD classification criteria
What is the diagnostic accuracy of other imaging modalities in people suspected of having SD?
- They do not recommend additional imaging modalities over and above USS in the routine assessment of SD
What is the diagnostic accuracy of major and minor salivary gland biopsy in people suspected of having SD?
- Consider a minor labial salivary gland biopsy to aid diagnosis in those with clinically suspected SD where the diagnosis cannot be made by clinical and serological features alone
- Minor (labial) SG biopsy—sensitivity 80–92%; specificity 88–97%— part of the most recent 2016 ACR/EULAR classification criteria when individuals are anti-Ro antibody negative and there is objective evidence of sicca affecting eyes and mouth
- Complication rates of minor salivary gland biopsy are low overall
- Parotid gland biopsy—sensitivity 78%; specificity 86%. Complication rates of parotid gland biopsy were low with no permanent sensory loss
What is the diagnostic accuracy of lacrimal gland biopsy in people suspected of having SD?
- There is currently insufficient evidence to routinely recommend lacrimal gland biopsy in SD
In people with confirmed SD, are there any measurable biomarkers that can predict development of lymphoma?
- Individuals with SD should be offered further investigation early if they present with new salivary gland swelling or other symptoms that might suggest the development of lymphoma
- Consider a minor labial salivary gland biopsy to provide additional prognostic data regarding lymphoma risk in both seronegative and seropositive individuals
- Predictors of future lymphoma development (may include):
- Low C3/C4 with low C4 being the strongest predictor
- Clinical evidence of salivary gland enlargement
- Clinical evidence of lymphadenopathy
- Cryoglobulinaemia
- Monoclonal gammopathy
- High focus score (>4)
In people with confirmed SD are there any measurable biomarkers that can predict disease progression or development of extraglandular disease?
- Baseline assessment of individuals with SD should include a thorough clinical and serological evaluation to inform the risk of development of extraglandular features and disease progression
What other investigations should routinely be undertaken to exclude common associated conditions, for example coeliac or thyroid disease?
- Be aware of and consider screening for commonly associated conditions, as guided by age and/or clinical presentation
- Recommend that the following additional investigations are undertaken at baseline, and repeated as clinically indicated, to detect comorbidities and associated autoimmune diseases:
- Vitamin D levels
- Thyroid function
- Liver function tests (and anti-mitochondrial antibodies if indicated)
- TTG
- Immunoglobulins and serum electrophoresis
- Serum bicarbonate
In people with SD who have sicca (dryness) symptoms of the eyes, what is the most clinically effective topical treatment?
- Advise regular use of a preservative free lubricating eye drop (e.g. 2–3 hourly)
- Autologous or allogeneic serum eye drops may be offered to individuals with ongoing symptoms despite maximal management with conventional eye drops
- Topical steroid eye drops, under ophthalmic supervision, may be offered short term to individuals with ongoing persistent inflammation despite maximal management with conventional eye drops
Other treatments for patients with SD who have sicca (dryness) symptoms of the eyes?
- Topical ciclosporin eye drops, under ophthalmic supervision, may be indicated for those with persistent surface inflammation despite maximal management with conventional eye drops
- Others studied: tacrolimus, Topical IL-1 antagonist, Lifitegrast, Rebamipide, Diquafosol
- Advise a heated eyelid compress for at least 10 min daily
- Lipiflow, IPL therapy and meibomian gland probing are not currently NHS funded as treatments within the UK. There is currently insufficient evidence to recommend their routine use. However, these procedures are safe with, in some cases, weak evidence of benefit in dry eye and individuals may decide to undergo these treatments in the private sector
- Those with dry-eye disease associated with meibomian gland dysfunction or blepharitis could be offered short-term treatment with oral or topical antibiotics with an anti-inflammatory action
- Individuals with dry-eye disease associated with meibomian gland dysfunction or blepharitis could be advised to use lipid containing eye drops or liposomal eye sprays as adjunctive treatment
- Punctal plugs are suitable in in certain circumstances, but they may make corneal surface inflammation worse in certain situations. Careful patient selection is important
- There is insufficient evidence to recommend androgen replacement therapy for dry-eye disease
In people with SD who have sicca (dryness) symptoms of the mouth, what is the most clinically effective topical treatment?
- Suggest saliva substitutes for symptomatic relief of oral dryness
SD patients who have sicca (dryness) symptoms outside the eyes and mouth, what is the most clinically effective topical treatment?
- Consider advising topical non-hormonal vaginal moisturizers plus oestrogen creams/pessaries in peri- or post-menopausal women with significant vaginal dryness
In people with SD who have sicca (dryness) symptoms, what is the most clinically effective stimulatory treatment?
- Consider a trial of pilocarpine (5 mg once daily increasing to 5 mg tds/qds) in those with significant ocular sicca symptoms with evidence of residual glandular function
- Consider a trial of pilocarpine (5 mg once daily increasing to 5 mg tds/qds) in those with significant oral sicca symptoms with evidence of residual glandular function
In people with SD what is the clinical effectiveness of treatments in comparison to each other or placebo for treating systemic disease?
- In those with significant fatigue and systemic symptoms consider a trial of HCQ for 6–12 months
- Systemic steroids may be used short term for specific indications but should not be offered routinely in the management of SD
- Conventional immunosuppressive drugs are not routinely recommended for use in SD outside of the treatment of specific systemic complications
- Biologic drugs are not currently recommended for use in SD outside of the treatment of specific systemic complications
- Intravenous immunoglobulins are not routinely recommended for use in SD outside of the treatment of specific systemic complications
- Colchicine may be helpful in SD presenting with specific systemic complications
What treatments are beneficial for recurrent parotitis in jSD?
- Treatment of parotitis in jSD (once infection and stone disease have been excluded) could include the following escalating therapies. A short course of NSAIDs or oral steroids combined with massage followed by washouts with saline or steroids. Consider anti-B-cell-targeted therapies in selected, refractory cases (2, C) (SOA 91%).
Is early treatment of hypergammaglobulinaemia or systemic disease more effective than delayed treatment at slowing disease progression?
- In SD with significant hypergammaglobulinemia consider a trial of HCQ for 6–12 month
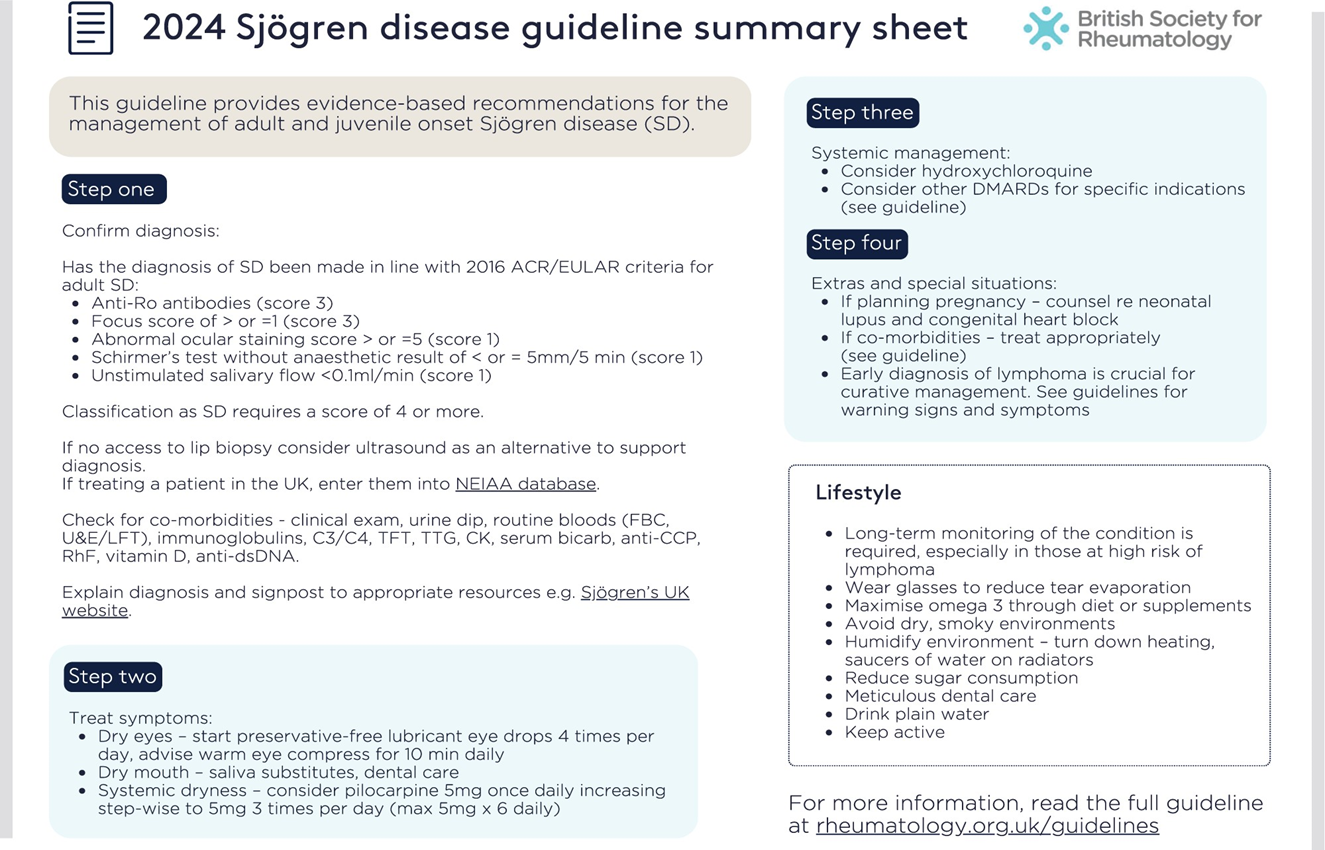
BSR Sjogren's Guideline Summary Sheet
Join The Discussion
For dry mouth, I see no mention of cevimeline. IMO this drug is very helpful and I have even seen patients intolerant of pilocarpine or with no response to pilocarpine, who have had improvement with cevimeline. As we know, the teeth in Sjogren's are a major target organ for damage and saliva is a major player in the health of the teeth. Note: I see on OpenEvidence that cevimeline is not approved in the UK.
also rutiximab is very helpful in SD with recurrent parotitis .
EN AQUELLOS CASO CON ESCLERITIS , HAY ESTUDIOS QUE RECOEIENDAN EL USO DE RITUXIMAB ASI COMO EN LA PATOLOGIA PULMNAOIR ASOCIADA A SJOGREN.
No existen estudios sobre el uso de rituximab para la escleritis en el síndrome de Sjögren, pero sí existen estudios sobre el uso de rituximab para el tratamiento de la escleritis.
https://www.aaojournal.org/article/S0161-6420(14)00398-4/abstract
https://pmc.ncbi.nlm.nih.gov/articles/PMC8364894/










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.