Humira Clobbers Biosimilars in Battle for Part D Coverage Save
Just about every Medicare Part D prescription drug plan on offer this year covers the original version of adalimumab (Humira), whereas only about half will pay for any of the several biosimilar versions currently approved, researchers found.
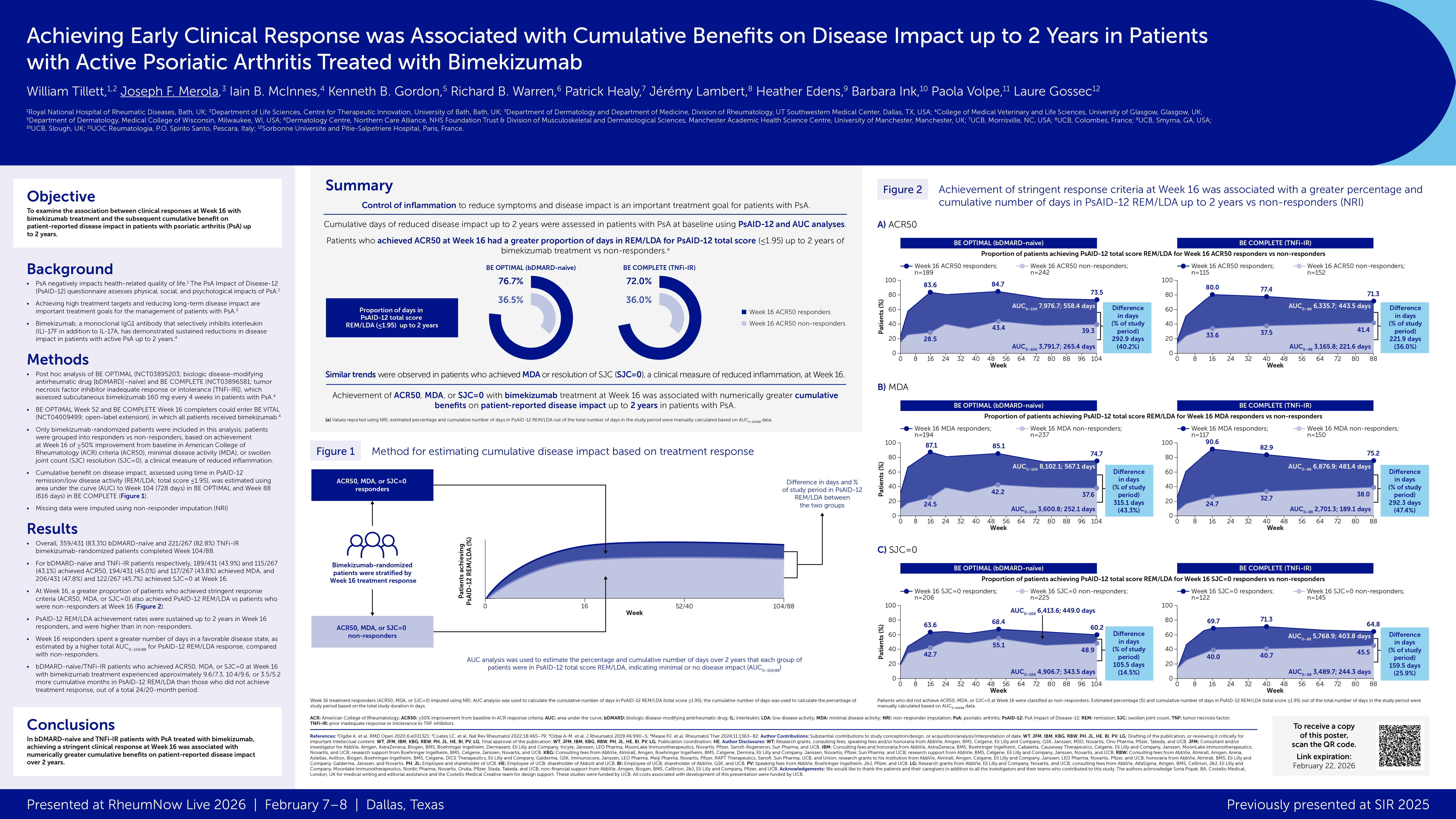
With 5,609 different Part D policies sold in the U.S. as of January 2024 (including standalone plans and those included in Medicare Advantage), 98.9% paid for Humira's high-concentration version, and nearly as many (98.7%) covered its low-concentration product, according to Matthew Klebanoff, MD, of the University of Pennsylvania in Philadelphia, and colleagues.
In contrast, just 53.4% of plans covered at least one biosimilar adalimumab product, the group reported in a JAMA research letter. These included about 60 plans that paid only for biosimilars, excluding Humira, which covered 2.1% of Part D enrollees.
Moreover, most of the biosimilars with substantial coverage came with a wholesale acquisition cost (the "list price") close to the $6,923 charged by Humira's maker, AbbVie, for a standard monthly supply. While two high-concentration biosimilars were priced below $1,500, they were covered by only 13% and 4.6% of plans, respectively, representing 9.9% and 5.3% of all Medicare Part D policyholders, the researchers noted.
The findings will be a disappointment to those who hoped the introduction of biosimilars would rein in the astronomical pricing typical of biologic drugs.
"[T]his study of formulary coverage helps explain limited uptake of adalimumab biosimilars," Klebanoff and colleagues wrote. "Subpar biosimilar adoption will not only undermine their potential to reduce spending but also may deter investments in biosimilar development. Policymakers should consider mandating Part D formulary coverage of biosimilars with substantially lower prices than originator biologics."
In fairness, the investigators noted that their study didn't examine so-called net pricing for adalimumab products, which reflect rebates and discounts from manufacturers. "By the end of 2023, Humira's annual net price decreased to $29,800, a 38% drop compared with $48,000 1 year prior, likely due to biosimilar competition," they acknowledged.
Still, they added, "biosimilars offer far greater potential savings: several adalimumab biosimilars have list prices that are less than half of Humira's net price."
Humira has long been the market leader for biologics in rheumatology, with nine approved indications ranging from rheumatoid arthritis (its initial approval in 2002) to inflammatory bowel disease and uveitis. An analysis published last year indicated that Medicare paid some $4.7 billion in 2021 for the drug.
Ten biosimilars for Humira have been approved since 2016. Three of these were also approved as interchangeable, meaning that patients may switch freely back and forth between original Humira and the biosimilar; however, Klebanoff and colleagues pointed out that two only come in low-concentration versions (40 mg/0.8 mL) which aren't prescribed nearly as often as the high-concentration product (40 mg/0.4 mL), and the third, which is available in the stronger formulation, was only approved this February.
Overall, only six of the biosimilars had any Part D coverage as of this January. The biosimilar with the broadest coverage, included in 50.7% of Part D formularies, was the low-concentration product Cyltezo (adalimumab-adbm, from Boehringer Ingelheim), with a list price of $6,576 for a monthly supply -- just 5% under Humira's.
Among high-concentration products, Sandoz's Hyrimoz (adalimumab-adaz) had the most coverage, included in 26.8% of plans, and it too listed for $6,576.
Another problem, the researchers found, was that few Part D plans sought to promote biosimilar uptake through "preferential tiering or utilization management," and "no plans used step therapy for any adalimumab product." In other spheres, insurers usually try to reduce their costs by putting cheaper drugs such as generics into the most favored category -- but this has not happened with adalimumab. Furthermore, no policies had looser requirements for prior authorization than those for Humira.
One limitation of the study was that while adalimumab biosimilars were nominally approved as long as 8 years ago, most were withheld from the market under agreements with AbbVie, which had alleged patent infringement. The very first approved biosimilar, in fact, was not sold in the U.S. until last year, which was also the case for several others.
Source Reference: Klebanoff MJ, et al "Formulary coverage of brand-name adalimumab and biosimilars across Medicare Part D plans" JAMA 2024; DOI: 10.1001/jama.2024.8917.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.