Lipids and Inflammation in Rheumatoid Arthritis Save
In the realm of chronic inflammation, lipid abnormalities are well-recognized as pivotal contributors to the progression and clinical manifestations of atherosclerosis. Particularly in rheumatoid arthritis (RA), a systemic autoimmune disorder, the immune response leads to the generation of inflammatory cytokines that profoundly alter lipid and lipoprotein metabolism. This review article delves into the latest research exploring the impact of inflammation on proatherogenic disorders of lipid and lipoprotein metabolism in RA patients, with a focus on proinflammatory cytokines.
Role of Proinflammatory Cytokines in Lipid and Lipoprotein Dysregulation
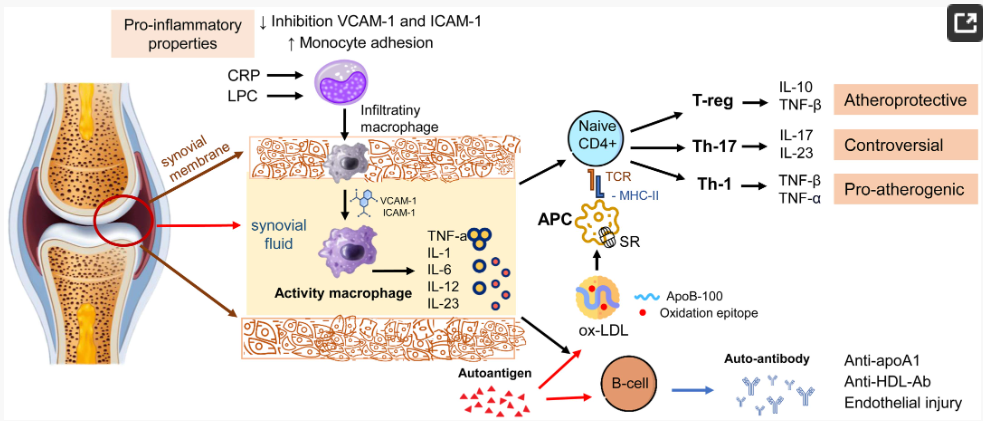
Inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), play crucial roles in orchestrating the inflammatory cascade in RA. These cytokines not only amplify the immune response but also influence lipid and lipoprotein profiles by modulating gene expression and metabolic pathways.
C-Reactive Protein (CRP)
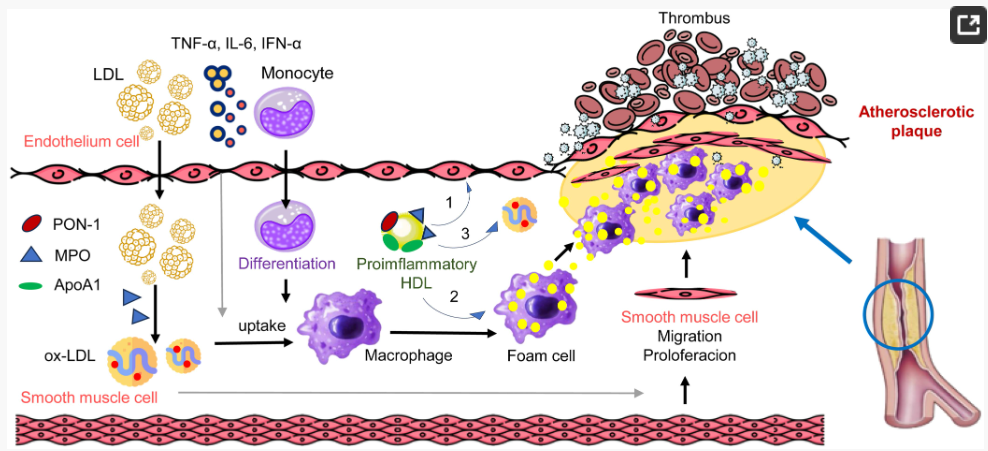
CRP, an acute-phase reactant, exhibits diverse atherogenic effects by modifying the behavior of low-density lipoproteins (LDL). Upon inflammatory stimuli, CRP can transform from its native pentameric form to a monomeric structure, which facilitates its binding to LDL. This CRP-mediated LDL opsonization promotes phagocytosis by macrophages, accelerating the development of atherosclerotic plaques. Moreover, CRP is associated with the generation of oxidized LDL, further contributing to vascular damage.
Myeloperoxidase (MPO)
MPO, another inflammatory mediator, produces reactive oxygen species (ROS) that impair HDL functionality. The oxidative modifications mediated by MPO alter the immunomodulatory and antioxidant properties of HDL, rendering it proinflammatory. Consequently, HDL fails to adequately remove excess cholesterol from cells, fostering atherosclerosis.
Lipid and Lipoprotein Profiles in RA Patients
Several studies have examined the blood lipid profiles of RA patients, highlighting notable differences compared to healthy controls. The concentrations of triglycerides, total cholesterol, and LDL-cholesterol (LDL-C) tend to be elevated in RA patients, whereas HDL-cholesterol (HDL-C) levels are often reduced. However, these general trends conceal significant heterogeneity within RA populations, suggesting that inflammation-specific lipid profiles could serve as valuable biomarkers for disease monitoring and risk assessment.
Subfractions of HDL
A detailed analysis of HDL subfractions reveals that the protective effects of HDL in RA are impaired. Specifically, the smaller, more atherogenic HDL3 subfraction tends to dominate over the larger, more cardioprotective HDL2 subfraction. Moreover, proinflammatory HDL complexes are enriched with acute-phase proteins and oxidized lipids, contributing to the proatherogenic phenotype.
LDL Dysfunction
LDL particles in RA patients exhibit alterations in size, density, and oxidative modifications. Small, dense LDL particles are more atherogenic than their larger counterparts, and oxidative modifications increase their ability to permeate endothelial barriers and induce inflammatory responses. These dysfunctional LDL particles accumulate in vessel walls, triggering atherosclerosis.
Impact on Cardiovascular Disease (CVD) Risk
The altered lipid and lipoprotein profiles in RA patients contribute significantly to their increased risk of CVD. In addition to traditional CVD risk factors, such as hypertension and diabetes, inflammation-mediated dyslipidemia in RA serves as an independent risk factor for CVD.
Future Directions
The understanding of the intricate interplay between inflammation and lipid metabolism in RA patients has profound implications for clinical practice. Future research should aim to elucidate the mechanisms underlying lipid and lipoprotein dysregulation in RA, identify novel biomarkers, and develop targeted therapies to address these dysfunctions. The successful implementation of such interventions has the potential to not only reduce CVD risk in RA patients but also improve their overall prognosis.
Conclusions
The effect of inflammation on proatherogenic disorders of lipid and lipoprotein metabolism in RA patients is a complex and multifaceted process. By investigating the mechanisms and clinical consequences of these disruptions, researchers can uncover novel strategies for preventing and treating CVD in this high-risk population.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.