Lupus Nephritis 2024 Guidelines Save
The ACR has published evidence-based and expert guidance for the screening, treatment, and management of lupus nephritis (LN). These are the same guidelines presented at ACR Convergence 2024.
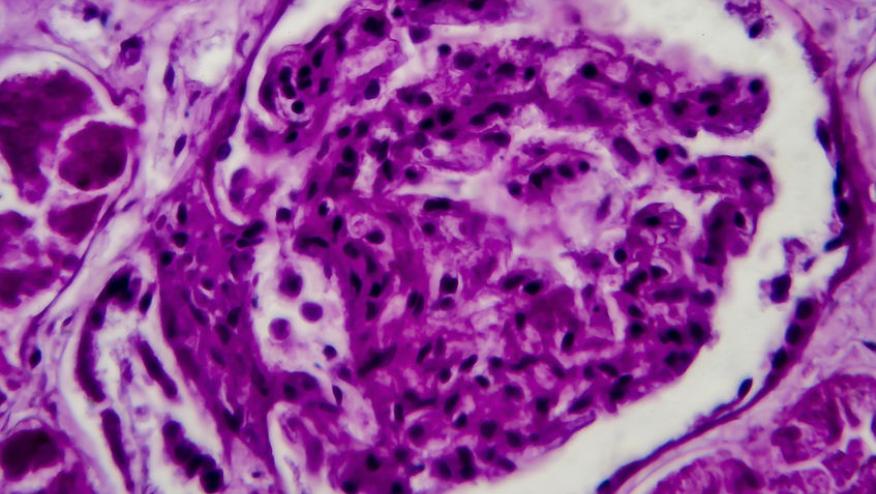
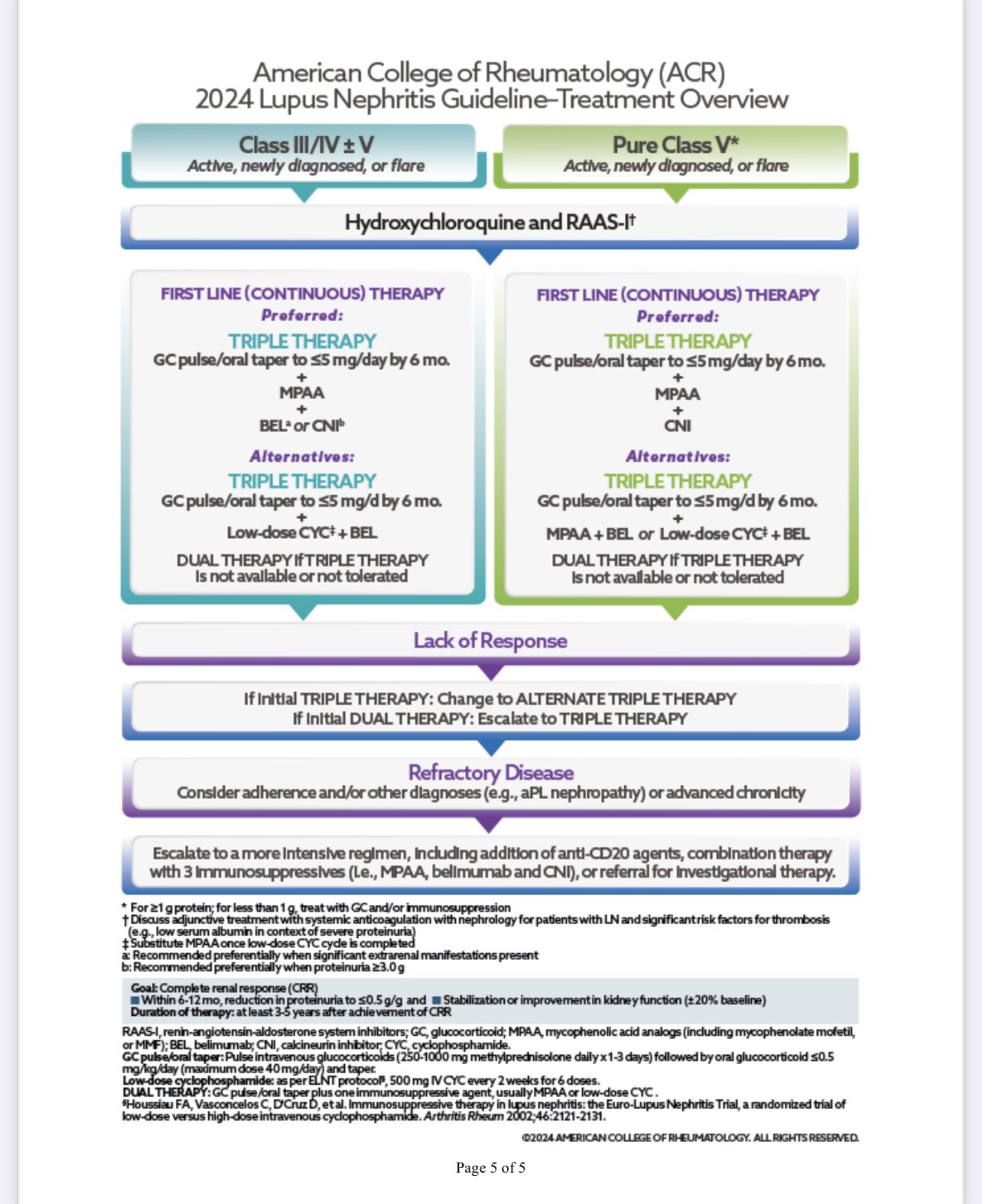
A multidisciplinary team of experts performed systematic literature reviews to address specific PICO questions on the screening, treatment, and management of lupus nephritis patients. Overall, there were 28 graded recommendations (7 strong, 21 conditional) and 13 ungraded, consensus-based good practice statements (GPS)for the screening and management of lupus nephritis. The diagnosis of lupus nephritis should be based on renal biopsy results. All LN patients should be on hydroxychloroquine plus a RAAS-I (renin-angiotensin-aldosterone system inhibitors including angiotensin converting enzyme inhibitors, angiotensin II receptor blockers, mineralocorticoid receptor antagonists). Initial therapy should include pulse glucocorticoids followed by oral glucocorticoid taper and two additional immunosuppressive agents for 3–5 years for those achieving complete renal response.
General Recommendations:
- LN therapy should be initiated as soon as possible after diagnosis.
- LN treatment should begin with intravenous glucocorticoids followed by oral
glucocorticoid (≤0.5 mg/kg/day prednisone, maximumdose40mg/day) taper and
also include triple therapy with:- Mycophenolic acid (MMF) plus belimumab or.
- MMF plus a calcineurin inhibitor (CNI) or
- Euro-Lupus Nephritis protocol of low-dose cyclophosphamide (CYC) plus
belimumab (with substitution of MPAA after completion of CYC)
- Pure Class V LN (≥1 g proteinuria) should also be treated with an initial steroid
regiment (above) and MMF plus a CNI. - The conditionally recommended duration of immunosuppressive therapy (beyond
hydroxychloroquine) for people with LN who achieve a complete renal response
(CRR) is 3-5 years.
Specific Recommendations:
- Screening: SLE patients should be screened for proteinuria at least every 6–12
months, OR when experiencing extra-renal flares. - Kidney Biopsy
- GPS: Prompt kidney biopsy should be performed in people with SLE when
LN is suspected. - SLE with proteinuria >0.5 g/g and/or impaired kidney function (not
otherwise explained), we conditionally recommend performing a
percutaneous kidney biopsy. - Treated LN in remission who present with suspected LN flare (increased
proteinuria, hematuria, and/or worsening kidney function), OR patients
with persistent ongoing or worsening proteinuria, hematuria, and/or
decreased kidney function, we conditionally recommend repeat
percutaneous kidney biopsy.
- GPS: Prompt kidney biopsy should be performed in people with SLE when
- Treatment of Active Class III/IV LN – good clinical practice (GPS)
- Prompt glucocorticoid treatment should be administered while awaiting a
kidney biopsy and the histopathology results. - Dosage of LN medications should be adjusted to GFR.
- Systemic anticoagulation should be considered in those with significant
risk factors for thrombosis (eg, low serum albumin in context of severe
proteinuria)
- Prompt glucocorticoid treatment should be administered while awaiting a
- Extra-renal manifestations: recommend a triple immunosuppressive therapy that
contains belimumab over a regimen containing a CNI. - Conditionally recommend a target MMF dose of 2–3 g/d (or equivalent).
- NON-RESPONSIVE OR REFRACTORY LN:
- GPS: Medication dose and patient adherence should be assessed.
- LN of any class with nonresponse (at least a partial renal response by
6–12 months) we conditionally recommend escalation of treatment:- Escalate from dual therapy to triple therapy (glucocorticoids,
followed by either MMF plus belimumab, MMF plus CNI, or CYC
plus belimumab).
- Escalate from dual therapy to triple therapy (glucocorticoids,
- For those failing triple therapy, consider alternative triple therapy or
addition of an anti-CD20 agent as a second immunosuppressive.
- MONITORING
- LN not achieving CRR, strongly recommend quantifying proteinuria at
least every 3 months. - LN in sustained clinical renal remission, strongly recommend quantifying
proteinuria every 3–6 months. - LN patients should have serum complement and anti-dsDNA antibody
levels measured at every clinic visit (but not more frequently than
monthly).
- LN not achieving CRR, strongly recommend quantifying proteinuria at
- End-Stage Kidney Disease (ESKD)
- ESKD with LN: recommend kidney transplantation over dialysis.
- LN who has progressive loss of kidney function and are nearing ESKD-
recommend preemptive kidney transplant over dialysis.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.