Pneumocystis Often Lethal in Dermatomyositis Save
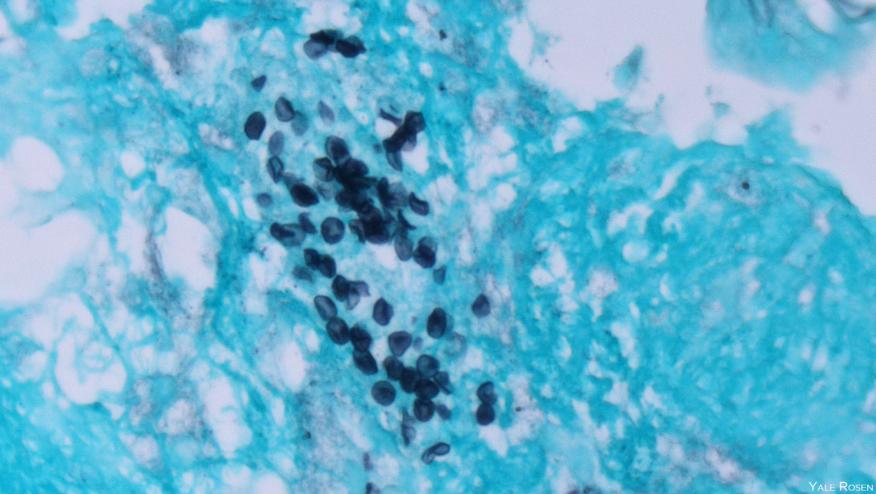
Patients with dermatomyositis who were positive for a myositis-specific antibody had a much higher incidence of and mortality associated with Pneumocystis jirovecii infection than patients with other antibody-negative idiopathic inflammatory myopathies, Chinese researchers found.
Among patients with dermatomyositis who were positive for the anti-melanoma differentiation-associated gene 5 antibody (MDA5), the prevalence of P. jirovecii pneumonia (PJP) was 7.5 per 100 person-years compared with only 0.7 per 100 person-years for those with MDA5-negative inflammatory myopathies (P<0.00001), said Qingran Yan, MD, and colleagues from Renji Hospital in Shanghai.
In addition, the hazard ratio for mortality associated with PJP in MDA5-positive dermatomyositis was 3.254 (95% CI 1.209-8.756) compared with patients who had PJP and other rheumatic diseases, the researchers reported online in Arthritis Research & Therapy.
Patients with rheumatic diseases who are treated with immunomodulating therapies are at risk for opportunistic infections such as PJP, with the risks highest for patients with dermatomyositis/polymyositis. Risks have also been reported as being elevated, though less so, for systemic lupus erythematosus, systemic sclerosis, and rheumatoid arthritis.
The myositis-specific antibody anti-MDA5 has long been recognized as a poor prognostic factor in dermatomyositis, characterized by rapidly progressive interstitial lung disease. Little is known, however, about the influence of antibody positivity on the incidence and mortality of PJP in patients with dermatomyositis.
Accordingly, the researchers reviewed cases of inflammatory myopathies seen at their hospital from 2017 to 2020, screening them for myositis-specific antibodies, and then examined outcomes for patients with rheumatic diseases who had confirmed cases of PJP.
A total of 463 cases of inflammatory myopathy were included; during a median follow-up of 18 months, there were 14 cases of PJP. Patients with PJP differed significantly from those without the infection, in that 85.7% were anti-MDA5 positive versus 33% (P<0.0001), more often had interstitial lung disease (92.9% vs 70.4%), and had lower overall lymphocyte and CD4+ T lymphocyte counts. PJP patients also had higher erythrocyte sedimentation rates and ferritin levels, and had greater prednisone exposure.
On a multivariate analysis, the only factors that were independently associated with PJP diagnosis were positivity for anti-MDA5 antibodies and low CD4+ T cell counts, the researchers found.
They then considered the influence of anti-MDA5 positivity on PJP mortality, and found that 30 patients with any rheumatic disease had been admitted to the hospital with PJP during the study period. Of these, 39.6% had MDA5-positive dermatomyositis, 22.7% had systemic lupus erythematosus, and one or two each had other diseases such as MDA5-negative inflammatory myositis, vasculitis, Sjogren's syndrome, and rheumatoid arthritis.
The PJP mortality rate for anti-MDA5-positive patients was significantly higher than for other rheumatic patients (83.3% vs 38.9%, P=0.016). On a univariate analysis, age, CD4 counts, and MDA5-positive dermatomyositis were identified as risk factors for 3-month mortality, and on a multivariate analysis, MDA5 positivity and lower CD4 T cell counts were independently associated with mortality.
However, while MDA5 dermatomyositis had a more than threefold higher hazard ratio for mortality, the hazard ratio for the CD4 T cell count was only 0.094 (95% CI 0.989-1).
Using a cutoff of six days after the first symptoms appeared for the initiation of anti-PJP treatment, better 1-year survival with early treatment was observed for patients with other rheumatic diseases (87.5% vs 40%, P=0.057), whereas survival was no better in MDA5 dermatomyositis if patients were treated promptly, the researchers reported.
The reasons patients with MDA5-positive dermatomyositis are so susceptible to PJP are not fully understood, the investigators noted. However, they said, "given the extremely high prevalence and poor outcome of interstitial lung disease in MDA5-positive dermatomyositis, we speculate that lung comorbidity may contribute to lethality" in these patients.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.