Rheums Speak: Changing Rheumatology Practices & Choices Save

RheumNow surveyed clinicians worldwide on how their rheumatology practice, treatment decisions, and career outlooks have changed over the past 20 years. 242 respondents (68% from the USA) shared their perspectives on the changing landscape of rheumatoid arthritis (RA) care, practice patterns, and professional development.
Two-thirds of respondents were in private practice, ~20% were from academic centers, 6% were fellows and <3% were advanced practice providers. Over 44% employ or work with 2 or more APPs (more in the US - 51%).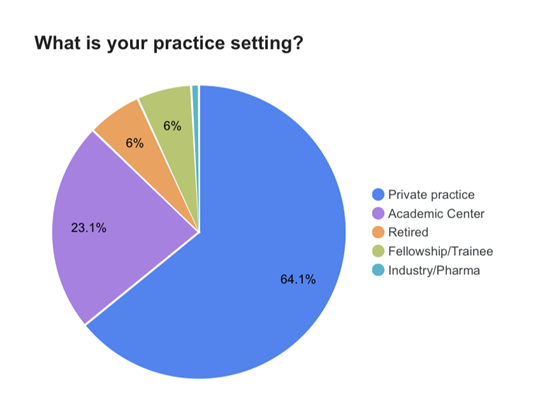
When asked about how their careers have evolved over time, 38% reported having greater knowledge and expertise, and 29% either are just starting out or growing their practice. Yet nearly 25% reported that they are “getting closer to burnout”, affirming the concerns of many - workforce contraction with the growth of arthritis and an aging population. 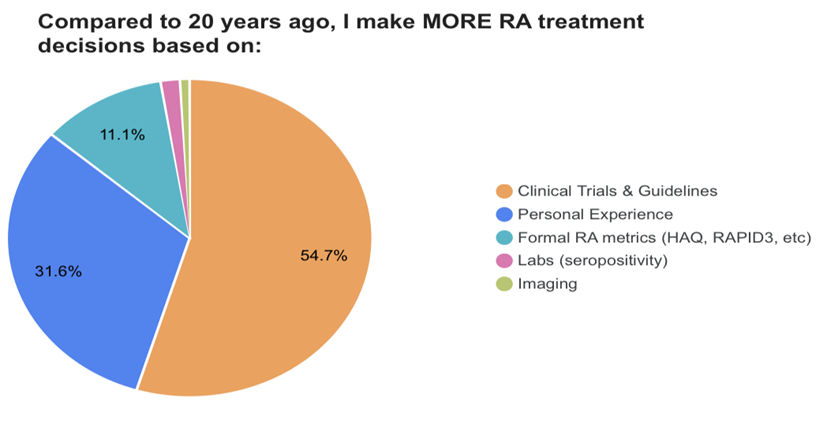
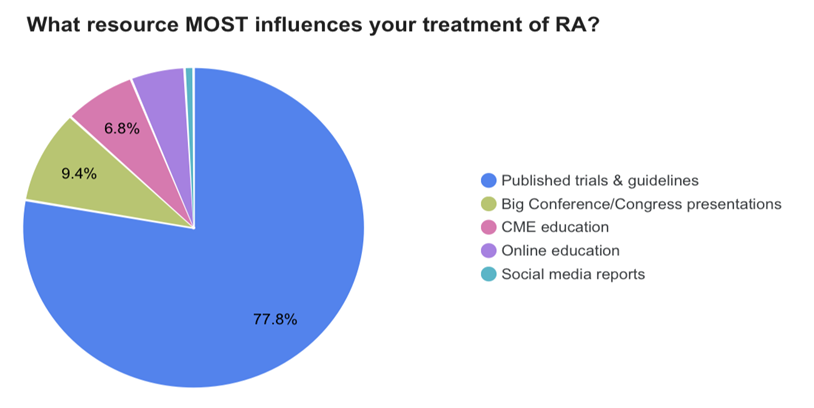
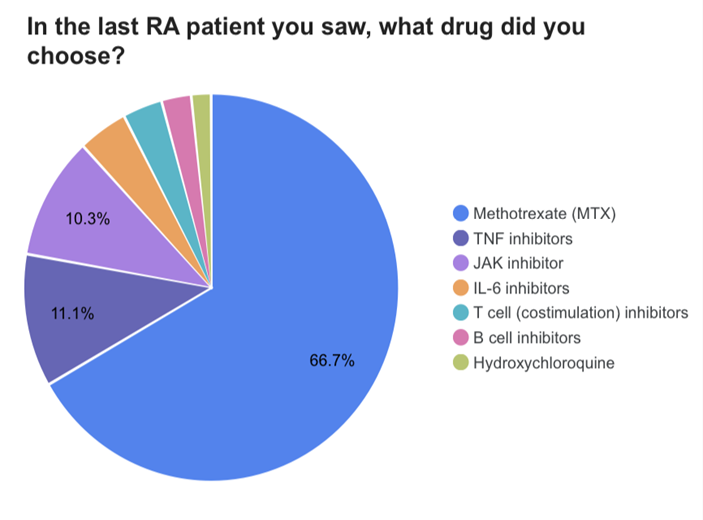
Respondents prefer to make their RA treatment decisions based on either published trials and guidelines (55%) or personal experience (32%). This is reinforced by 78% claiming to rely on published clinical trials and guidelines, more so than conferences (9%) or CME education (6.8%). With trials, literature and guidelines at the forefront, they indicate a traditional conservative approach noting that the last drug they prescribed for RA was either methotrexate (67%), TNF (11%) or JAK (10%) inhibitors, and only 10% prescribed a non-TNF biologic (IL-6 inhibitor, abatacept or rituximab).
Only 11% make RA treatment decisions based on formal metrics; suggesting treat-to-target is not employed by most. Yet, when they assess RA patients, 82% claim to rely on swollen joint counts (38%), CDAI (31%) or RAPID3 (13%). 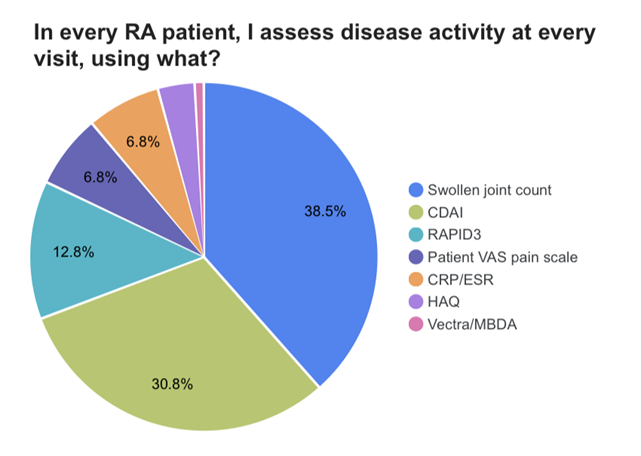
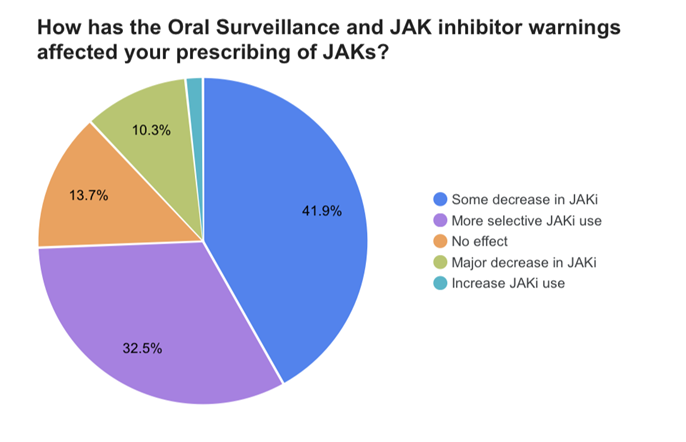
Since the release of regulatory safety warnings for JAK inhibitors (prompted by the Oral Surveillance trial), the vast majority (88%) report a decrease in JAK inhibitor prescribing; 42% with some decrease (more in US - 50%), a major decrease in 10% and more selective use in 32%.
Comorbidity Concerns
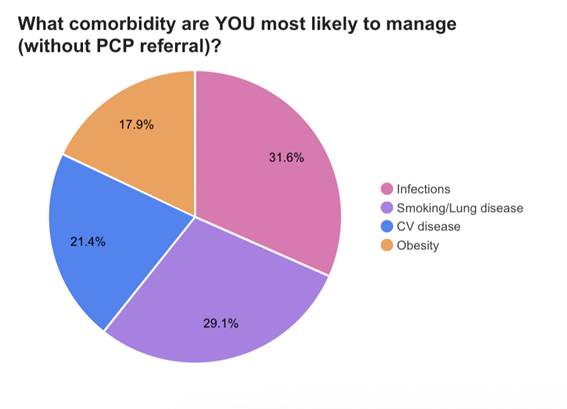
Half of the respondents worry most about CV disease (50%) in their RA patients; followed by 22% infection and 17% lung disease. Rheum respondents were equally split on which comorbidity they would be most apt to manage without referring to a primary care provider.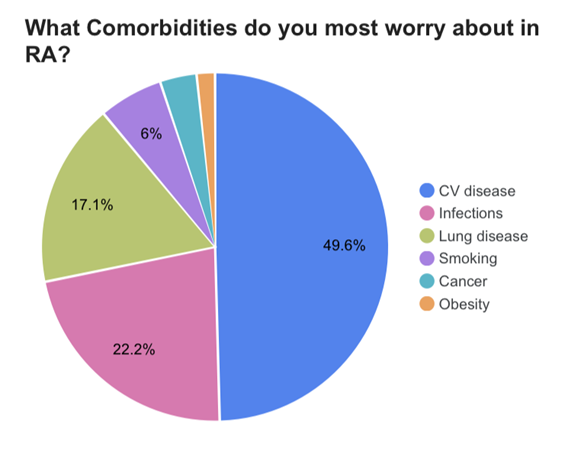
This series of surveys on RA, Biologics and DMARDs is sponsored by Bristol Myers Squibb










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.