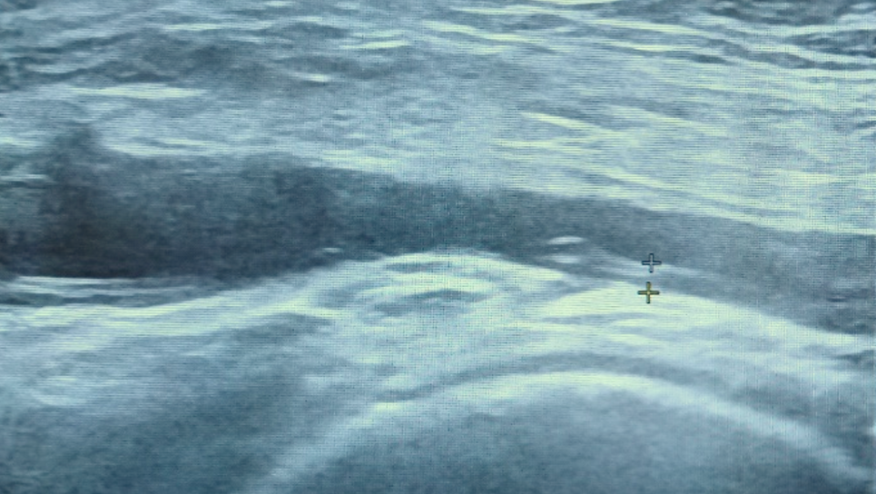
Subclinical vasculitis in polymyalgia rheumatica Save
For a long time polymyalgia rheumatica (PMR) has been an underinvestigated disease. This is changing with new possibilities to make a more accurate diagnosis with imaging as well as new therapies for treatment resistant disease.
Frequent use of vascular ultrasonography and positron emission tomography and computed tomography (PET/CT) increase the possibility of encountering a patient with solely symptoms of PMR (no cranial symptoms), but giant cell arteritis (GCA) confirmed with imaging. This group of PMR patients with so-called subclinical large vasculitis represents a clinical challenge.
It is well known that PMR often co-exists with GCA and recent meta-analyses have demonstrated that subclinical GCA as well as GCA in general may be present in more than 20% of patients with PMR. Most of these studies evaluated PMR patients from tertiary centers introducing a selection bias towards a higher proportion of patients with GCA. Therefore, the real proportion of PMR patients with subclinical GCA may be considerably lower, but nevertheless represent a common challenge in routine care for PMR patients.
Do we need to screen all PMR patients without cranial symptoms for GCA at the time of diagnosis?
We know that some difficult to treat PMR patients have an underlying GCA, and may need treatment with glucocorticoids using GCA doses. Identifying these patients at the time of diagnosis with imaging will probably result in a better disease course.
However, the other side of the coin is that we might overtreat some patients with subclinical PMR that previously responded well to glucocorticoids in PMR doses. In other words, the prognosis and optimal glucocorticoid dose for these patients are currently unknown, but they may be at greater risk of relapse. Personally, I perform vascular ultrasonography in my patients with PMR, but it is not mandatory at our department. I also treat these patients with glucocorticoids in GCA doses. Hopefully we will have more evidence to back up our clinical practice in the future. In addition, it is worth mentioning that routine evaluation for subclinical GCA in patients with PMR is currently not possible in many vasculitis centers. Only a limited number of rheumatologists can perform vascular ultrasound in many countries and especially PET/CT has limitations (high cost, limited availability, and incidental findings requiring additional investigation).
Should we evaluate all PMR patients regularly for GCA with imaging during the disease course?
Although I have seen many PMR patients where GCA was ruled out at diagnosis and later confirmed during the disease course, no study has actually evaluated the incidence rate using imaging both at the initial PMR diagnosis and at a later subclinical GCA diagnosis. Therefore, the incidence rate as well as the clinical implication remains unknown, and I only perform imaging for GCA during the PMR disease course in cases of clinical GCA suspicion (e.g., treatment resistant disease or cranial symptoms).
In conclusion, subclinical GCA in patients with PMR represents a common clinical challenge and much more evidence are needed. Currently there is insufficient evidence to recommend screening of all PMR patients for subclinical GCA with imaging. I treat patients with subclinical GCA the same way as patients with GCA, but this may change as our knowledge improves in the future.
(Legend for top image: US of the axillary artery of a patient with polymyalgia rheumatica without cranial symptoms. Three years after diagnosis at the third relapse after tapering glucocorticoids.)
Join The Discussion
Great commentary and while I am not a neuro radiologist those snow ball corpus lesions look very Susac like!!!
Len










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.