Do JAK Inhibitors Increase the Risk of Venous Thromboembolic Events? Save
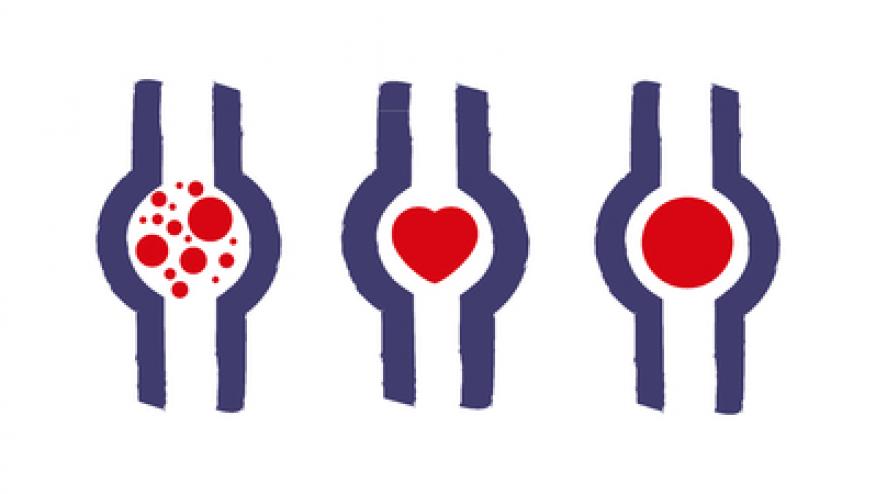
Drug Safety has published a systematic review of the FDA’s Adverse Event Reporting System (FAERS) and finds numerous reports of thromboembolic adverse events (AEs) associated with two currently marketed Janus kinase (JAK) inhibitors, tofacitinib (Xeljanz) and ruxolitinib (Jakafi). (Citation source: https://buff.ly/2zXyY2X)
The issue was recently brought to the forefront when the FDA issued a complete response letter to Lilly because of an "imbalance in thromboembolic events" (VTE) seen with their JAK 1 inhibitor, baricitinib (but not with placebo) in their rheumatoid arthritis (RA) development trials.
Baricitinib is currently approved in the European Union, Japan, Switzerland and Kuwait, where the small risk of thromboembolic events is listed under drug safety in the product label.
There is no warning or risk of thromboembolic events in the current product label for either tofacitinib (Xeljanz) and ruxolitinib (Jakafi).
Multiple reports have shown that RA patients (and many other autoimmune and inflammatory diseases) have a higher risk of VTE (http://buff.ly/2tAHGRO) that is unrelated to the use of DMARDs or TNF inhibitors. Multiple studies have shown that the risk of VTE in RA is about 5-6 VTE per 1000 person years. (http://buff.ly/2tAEu8t).
To further assess the risk with tofacitinib and ruxolitinib, researchers queried the Medwatch FEARS database and only included those VTE events where the drug was listed as the “primary suspect” for the AE.
The following events were identified:
- Pulmonary thrombosis: 18 unique cases for tofacitinib (16 resulted in hospitalization), 9 for ruxolitinib (all resulted in hospitalization, and 2 deaths are suspected to be linked), 3 for extended-release tofacitinib (all resulted in hospitalization).
- Pulmonary embolism: 36 unique cases for tofacitinib (25 resulted in hospitalization, 4 in death, 5 in life-threatening events), 55 for ruxolitinib (36 resulted in hospitalization, 12 in death, 1 in disability, 5 in life-threatening events), and 3 for extended-release tofacitinib (all resulted in hospitalization).
- Portal vein thrombosis: 11 unique cases were reported for ruxolitinib (9 cases resulted in hospitalization and 2 in death).
- Deep vein thrombosis: 18 unique cases for tofacitinib (11 resulted in hospitalization, 3 in death, 1 in disability, and 1 in a life-threatening event), 40 for ruxolitinib (28 resulted in hospitalization, 10 in death, 1 in disability, and 3 in life-threatening events), and 1 for extended-release tofacitinib that did not have a specified outcome.
- Thrombosis: 43 unique cases for tofacitinib (19 resulted in hospitalization, 2 in death, and 1 in a life-threatening event), 75 for ruxolitinib (43 resulted in hospitalization, 11 in death, 1 in disability, and 2 in life-threatening events), and 5 for extended-release tofacitinib (4 resulted in hospitalization).
Of course there is no event rate here and there is no denominator to know if this is high, low or expected given the patient and disease treated. Hence its curious that these many events were identified post-marketing but not during the drug development for ruxolitinib and tofacitinib.
At the 2017 American College of Rheumatology annual meeting, there were numerous studies that addressed this issue:
- Genovese et al (Abst #511) showed the baricitinib risk for DVT/PE was 12/1000 Pt years in the first 6 mos and with long term follow up was 5-6 per 1000 PY
- Mease et al (Abst #16L) reviewed the risk of VTE in the RA, psoriasis, psoriatic arthritis and ulcerative colitis programs and found no VTE events with psoriasis or ulcerative colitis, but noted few events with both 5 mg and 10 mg tofacitinib that appeared to be less than that seen with methotrexate alone.
The risk of VTE with RA and like disorders remains a rare and possible association. Whether this risk is augmented by JAK inhibitors remains to be seen. Hopefully the FDA will further analyze and clarify this issue for all JAK inhibitors.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.