Gastrointestinal Perforation Risk increased for Tofacitinib and Tocilizumab Save
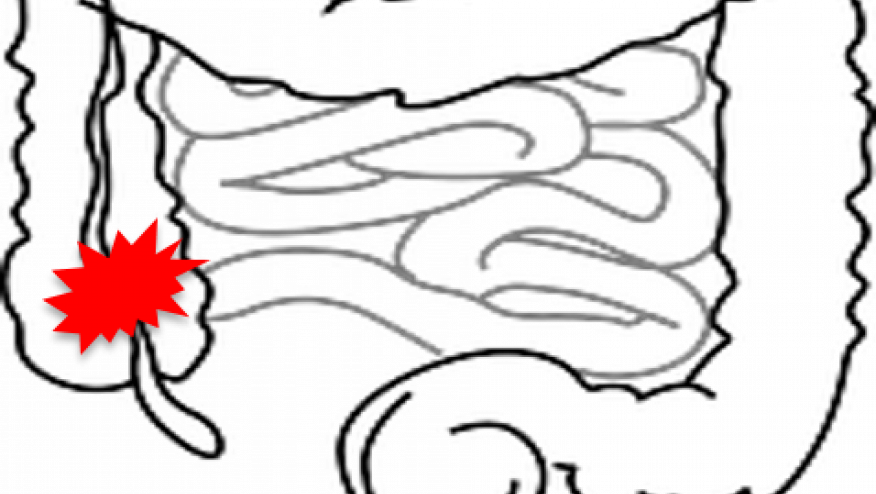
Gastrointestinal perforations (GIP) are not historically believed to be a common or uncommon complication. Hence, when this was noted in the tocilizumab (TCZ) and tofacitinib (TOFA) developmental trials, it was a curious if not perplexing finding. The product label for both TCZ and TOFA warns of GIP in those at risk, and noted these to be rare events (0.26 per 100 patient-years in the TCZ trials).
What we have since learned from the research of Dr. Jeff Curtis and colleagues is that the risk is more closely linked to steroid use, age and those with a prior history of diverticulitis, but not diverticulosis, nor these newer non-TNF biologics.
A recent real-world analysis by Xie, Yun, Bernatsky and Curtis has shown that the risk of GIP, especially lower GIP, may be higher with TCZ and TOFA.
Using claims data from 2006-2014, RA patients without prior GIP were analyzed for incident GIP within hospitalization. Among 167,109 RA patients, treatments included 4,755 who initiated tofacitinib, 11,705 tocilizumab, 115,044 anti-tumor necrosis factor (TNFi), 31,214 abatacept, and 4,391 rituximab.
Most perforations occurred in the lower GI tract, such that the incidence of lower GIP was 1.29 for tofacitinib, 1.26 tocilizumab, 0.76 abatacept, 0.73 rituximab, and 0.46 with the TNFi. Lower tract GIP risk was significantly elevated for both TCZ and TOFA patients compared to those on TNFi. Adjusted hazard ratios (HRs) were TCZ 2.55 (95%CI 1.33-4.88), TOFA 3.24 (95%CI 1.05-10.04).
Significant risk factors included older age (HRs=1.16 per 5 years), diverticulitis/other gastrointestinal conditions (HR=3.25), and prednisone use >7.5mg/day (HR=2.24).
Reasons for this doubling of risk for lower-tract gastrointestinal perforation with tocilizumab and tofacitinib is unclear. The higher rate noted with TOFA and TCZ suggests that either these events are more common in the way in which these drugs are used or that the risk may be tied to IL-6 inhibition. Whereas TCZ is specific for the IL-6 receptor, the mechanisms underlying the efficacy and toxicity of the JAK inhibitor is more pleotropic, but does include the ability to inhibit IL-6. Other side effect similarities between the 2 agents include effects on hepatic enzymes, cholesterol metabolism, cytopenias and a very low risk of tuberculosis (compared to the TNFi agents).










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.