Best of 2024: Consensus Statements on Vitamin D Save

This article originally appeared May 15, 2024, and is being shared again as our "Best of 2024". Enjoy!
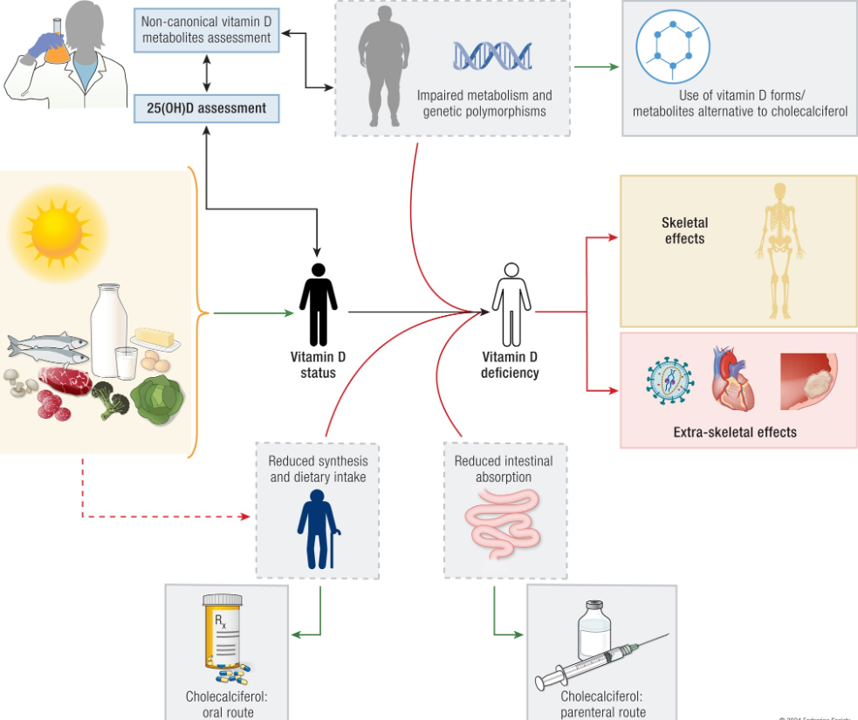
The “Controversies in Vitamin D” International Conference has published their proceedings on vitamin D metabolism, assessment, actions, and supplementation. Interestingly, optimal levels of 25-hydroxy vitamin D (25(OH)D) are still being debated.
Varying recommendations by society with significant differences in assays.
Vitamin D's extraskeletal effects has led to clinical trials on cancer, cardiovascular risk, respiratory effects, autoimmune diseases, diabetes, and mortality. They claim that negative results are likely due to enrollment of vitamin D-replete individuals, but there are some post hoc analyses suggesting some potential benefits in reducing cancer, autoimmune diseases, cardiovascular events, and diabetes.
Oral administration of vitamin D is the preferred route. Parenteral administration is reserved for specific clinical situations.
Take home points:
- Total serum 25-hydroxyvitamin D concentration is the biomarker of vitamin D status, but assay results may vary
- Vitamin D deficiency reduces intestinal calcium absorption leading to secondary hyperparathyroidism, bone loss, and increased risk of fractures in older adults. In these instances, clinical trials show that vitamin D and calcium, can decrease hip and other fractures in nursing home residents
- Post hoc analyses of recent mega trials on extraskeletal effects of vitamin D suggest a link between vitamin D status and immune system and development of type 2 diabetes mellitus.
- Oral cholecalciferol (vitamin D3) remains the preferred form of vitamin D for supplementation, while other vitamin D analogues (e.g., calcifediol, calcitriol, alfacalcidol) may be used in specific conditions
Screening and Testing for Vitamin D
- It is well recognized that serum 25(OH)D levels vary by season
- Where there is a low prevalence of vitamin D deficiency, screening of the general population is not cost-effective. There is little evidence for the utility and cost-effectiveness of testing for 25(OH)D deficiency in the general population
- Prioritized screening should be used for high-risk groups
- Screening is indicated in high risk populations:
- parathyroid disorders, liver disease, obesity, bariatric surgery, working long hours indoors, dark-skinned individuals, chronic disease patients, etc.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.