Biomarker Predicts Survival in Autoimmune Lung Disease Save
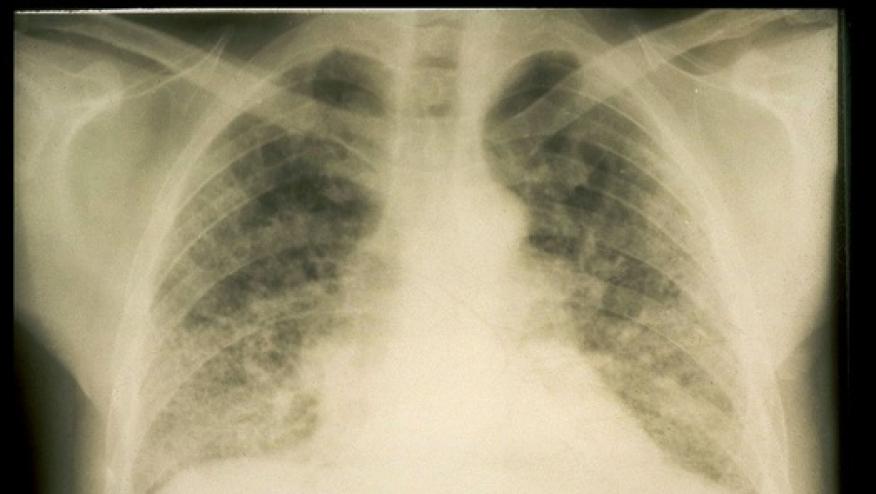
One major subgroup of patients with interstitial lung disease (ILD) arising from polymyositis/dermatomyositis (PM/DM) survived significantly longer when serum levels of interferon-λ3 were relatively low, researchers found.
Some 70% of patients in this subgroup showing serum interferon-λ3 above 120 pg/mL at baseline -- the median among the 52 patients in this analysis -- remained alive 6 months later, compared with 90% of those with lower levels (P=0.049), according to Tomoyuki Fujisawa, MD, PhD, of Hamamatsu University in Japan, and colleagues. The survival difference was even greater in a separate, smaller cohort.
This PM/DM-ILD subgroup is defined by the presence of anti-melanoma differentiation-associated gene 5 (MDA5) autoantibodies; previous studies had shown that this form of the disease is clinically distinct from others, Fujisawa and colleagues explained in their report appearing in Arthritis & Rheumatology.
In their new study, involving a total of 221 PM/DM-ILD patients, elevated interferon-λ3 was seen only in the roughly 35% with anti-MDA5 antibodies. Survival in this group was worst among those older than 53 and with partial arterial oxygen pressure (PaO2) below 75 mm Hg.
Fujisawa's group got interested in interferon-λ3 in the context of PM/DM-ILD after seeing numerous reports that this cytokine was elevated in a variety of other autoimmune diseases including rheumatoid arthritis, lupus, and systemic sclerosis. Because it's believed to modulate immune activity at the epithelial barrier, it made sense that it might play a role in autoimmune ILD. However, no previous studies had examined interferon-λ3 in PM/DM patients.
The researchers initially analyzed a cohort of 155 PM/DM patients with ILD who had been treated at Hamamatsu University's medical center. Of these, 52 were positive for anti-MDA5 antibodies; most of the rest instead carried antibodies against aminoacyl-tRNA synthetase (ARS). Median follow-up after baseline testing was 49 months. Fujisawa and colleagues also examined a separate group (validation cohort) of 66 PM/DM-ILD patients, among whom 41% were positive for anti-MDA5 antibodies and who had median follow-up of 30 months.
Median patient age was 59 across both cohorts, and two-thirds were women. The disease was considered acute in some 30%, subacute in 30%, and chronic in 40%.
Interestingly, all the deaths in both cohorts occurred within the first 5 months of follow-up, even though observation continued for several years in both groups. Just under 20% of the validation cohort with interferon-λ3 levels below 120 pg/mL at baseline died, compared with fully half of those with higher levels. None of the patients with anti-ARS antibodies or those lacking any known autoantibodies had detectable levels of interferon-λ3.
Each 10-pg/mL increment in interferon-λ3 was associated with a 4.5% increase in mortality risk after adjustment for covariates (P=0.01). Age was also a factor, with a 9.5% increase in mortality for each additional year of age (P=0.004).
Among 17 patients older than 53, with interferon-λ3 at 120 pg/mL or higher, and PaO2 below 75 mm Hg, almost 80% died within 5 months. In contrast, mortality among patients with two of these characteristics but not all three (n=26) was about 25%.
Fujisawa and colleagues refrained from speculating on whether interferon-λ3 might represent a therapeutic target as well as a diagnostic marker. They did, however, call for prospective studies to better understand the connection between interferon-λ3 and ILD and to confirm the biomarker's potential as a clinically useful prognostic indicator. Further research could also identify the most appropriate cutoff values for decision-making.
Limitations to the study included the relatively small numbers of patients and the lack of testing for other possible influences such as other interferon species. Also, interferon-λ3 levels were measured only once in each patient, and thus the potential for variability over time was not examined.
Source Reference: Fukada A, et al "Prognostic role of interferon-lambda 3 in anti-MDA5–positive dermatomyositis-associated ILD" Arthritis Rheumatol 2023; DOI: 10.1002/art.42785.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.