Consensus Recommendations on JAK Inhibitor Use Save
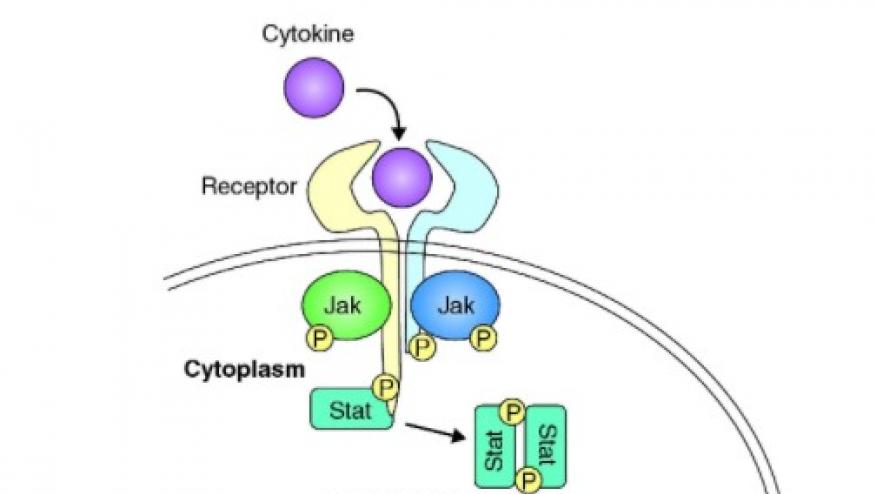
A steering committee and task force was convened to develop recommendations for the use of Janus kinase (JAK) inhibitors in the treatment of immune-mediated inflammatory diseases (IMID).
The steering committee of 15 experts in JAK inhibitors, inflammatory and rheumatic diseases was joined by an expanded Task Force of 14 additional individuals that included two patient research partners, a health professional, dermatologist, gastroenterologist, hematologist, an infectious disease specialist and a fellow. They utilized EULAR standard operating procedures for the development of recommendations. After developing the research questions and review of the literature, they formulated the general principles and recommendations (points of consideration). These were published in Annals of Rheumatic Disease.
Overall they put forth 4 general principles and 26 points for consideration addressing indications, treatment dose and comedication, contraindications, pretreatment screening and risks, laboratory and clinical follow-up examinations, and adverse events. Strength of evidence ranged between 8.8 and 9.9 on a 10-point scale.
4 General Principles
- Initiation of JAK-inhibitor therapy and treat to target should be achieved based on a shared decision between the patient and the medical specialist
- Therapeutic approaches to treating patients with chronic inflammatory conditions should be in line with international and national recommendations
- The points to consider when initiating JAK-inhibitor therapy do not provide information on when JAK-inhibitors should be used in the treatment algorithm, but rather attempt to assist the clinician once the decision to prescribe a JAK inhibitor has been made.
- These points to consider address specific (but not all) aspects related to the application of JAK-inhibitor therapy and the clinician should additionally refer to the disease-specific product information.
26 Points for Consideration
Indications
- Patients with immune mediated inflammatory diseases (IMIDs) who have failed prior conventional and/or biological therapies; as of 2019, these include rheumatoid arthritis (RA), psoriatic arthritis (PsA) and ulcerative colitis (UC).
- Currently, there is no direct evidence of superiority regarding efficacy or safety of one JAK-inhibitor over another one
Treatment dose and comedications in different IMIDs
- Use the dose recommended for the specific disease
- Consider dose adjustments in patients with higher age (>70 years), significantly impaired renal or hepatic function and/or risk of drug-interactions, or as a result of other comorbidities, as per individual product information.
- Regarding comedication, follow specific recommendations for the respective disease; in RA consider adding a JAK inhibitor to continued csDMARDs, if the patient tolerates the csDMARD1aA929.
- Consider dose reduction of the JAK inhibitor in RA patients in sustained CDAI or Boolean remission on background csDMARDs.
Contraindications
- Severe active (or chronic) infections, including TB and opportunistic infections.
- Current malignancies
- Severe organ dysfunction, such as severe hepatic disease (Child-Pugh C) or severe renal disease.
- Pregnancy and lactation
- Recurrent VTE (unless anticoagulated)
Pre-treatment screening and risks
- Patient history and physical examination.
- Routine laboratory testing (full and differential blood counts, liver tests (transaminases), renal function; lipid levels at approximately 3 months after initiation of therapy (and possibly at baseline unless measured within the last 12 months); no CPK testing recommended
- Hepatitis B testing (hepatitis B surface antigen, hepatitis B surface antibody, hepatitis B core antibody, and with/without HBV DNA testing as discussed in text). Hepatitis C testing (hepatitis C antibody, with HCV RNA testing if antibody positive)
- Human immunodeficiency virus testing in high-risk populations
- TB screening as per national guidelines
- Assess and update vaccination status.
- Consider risk factors for VTE, especially a past history of VTE
Adverse events
- Serious infections (similar to bDMARDs), opportunistic infections including TB, Herpes zoster* (increased rates compared to bDMARDs); the risk of infectious events can be lowered with reduction or elimination of concomitant glucocorticoid use.
- Rates of malignancy do not appear elevated with JAK inhibition, although the risk of NMSC may be elevated.
- Lymphopenia, thrombocytopenia, neutropenia, anaemia may occur.
- An increased risk of VTE has been reported in a safety trial of RA among patients using 10 mg two times a day tofacitinib and within the placebo-controlled trial period of baricitinib in patients with RA.
- Elevations of CPK are noted with JAK inhibitors but have not been associated with clinical events. Elevations of creatinine have been noted with JAK inhibitors but have not been associated with renal failure or hypertension
Laboratory and clinical monitoring during follow-up
- Minimal laboratory monitoring: full and differential blood counts and liver transaminase tests at 1 and 3 months and then periodically, such as every 3 months; lipid levels only at month
- Annual skin examination (for detection of skin cancer)
- Evaluate response using validated, disease-specific measures of disease activity; for evaluation and definition of response, be aware that CRP and ESR may be reduced independently of reduction of disease activity and possibly even in infections.
Disclaimer
This is not a EULAR guideline document or activity. This research was funded by AbbVie and Eli Lilly and Company.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.