Epigenetics and Autoimmune Skin Disease Save
The central dogma proposed that genetic information predominantly transfers from DNA to RNA during gene expression to make a functional product protein. This absolute theory has been debunked because of the influence of the environment on how genes are transcribed. According to the human genome sequencing and analysis, an extremely complex regulatory mechanism is required to regulate gene expression inside the human body, resulting in the activation or inhibition of pathways or molecules that may contribute to health or illness. Epigenetic processes partly account for this regulation. Epigenetics is the structural modification of chromosomal areas to record, signal, or maintain changed activity levels. Since the word “epi” means “above,” epigenetics literally means “above genetics.” Over the past decades, the study of epigenetics has blossomed, exposing an astonishing level of complexity in the way genetic information is stored and retrieved in eukaryotes. The most important epigenetic mechanisms are DNA methylation, histone modification, and noncoding RNAs. This review, in Frontiers of Medicine, discusses the most recent findings regarding the function of epigenetic mechanisms in autoimmune-related skin disorders, including systemic lupus erythematosus, bullous skin diseases, psoriasis, and systemic sclerosis
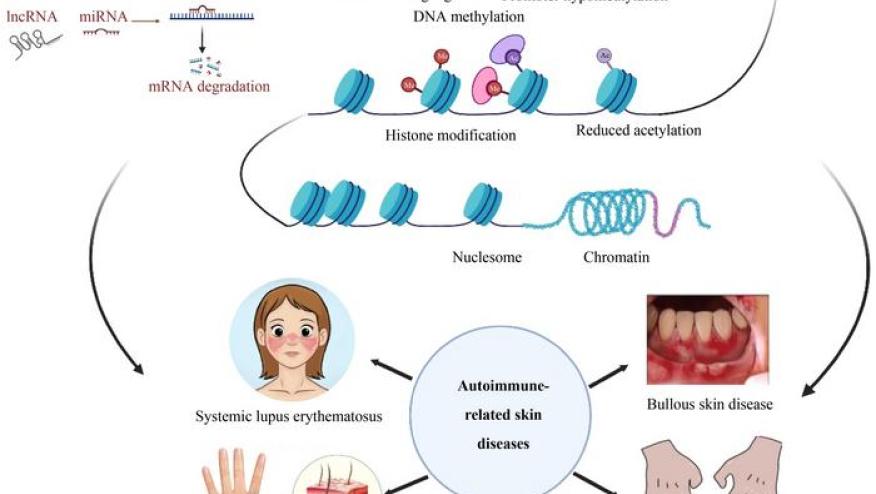
Autoimmunity is a pathological disease in which immune cells cannot recognize self-antigens; thus, they attack self-tissues and organs, causing inflammation and organ damage, including the skin. As the body’s largest organ, the skin can be affected by overactivated immune cells and autoantibody production. The pathogenetic mechanisms related to autoimmunity in skin diseases remain poorly understood. However, these diseases are widely believed to result from the interaction of genetic susceptibility and environmental stimuli. Although several associated risk loci have been found via genome-wide association analysis, the high prevalence of discordance in the occurrence of autoimmune diseases in homozygous twins cannot fully be explained by genetic factors. A growing body of research has demonstrated that epigenetic modifications have a critical role in the onset and development of autoimmune-related skin diseases. Multiple forms of epigenetic modifications modulate gene expression. The three major features are DNA methylation, histone modifications, and noncoding RNAs (ncRNAs). These epigenetic modifications may substantially affect cell function, defining the phenotype of each cell. Therefore, this review summarizes the most important and current findings of epigenetic contributions to autoimmune diseases in dermatology, including systemic lupus erythematosus (SLE), bullous skin diseases, psoriasis, and systemic sclerosis (SSc) (Fig.1).
Given the development of potent new techniques, studies on epigenetics published over the last few decades have identified multiple epigenetic aberrations in various autoimmune-related skin diseases. These epigenetic alterations have a remarkable impact on the four principal autoimmune-related skin disorders covered in this study, demonstrating a close relationship between epigenetic dysregulation and the pathogenesis of autoimmune-related skin disorders. Specific epigenetic dysregulations in autoimmune diseases may serve as possible disease biomarkers. One of our earlier studies demonstrated that the IFI44L promoter methylation level is a very sensitive and specific diagnostic biomarker for SLE. This research finding was successfully translated into clinical application. Instead of pyrosequencing IFI44L DNA methylation levels, our group has established a high-resolution melting technique that can be quickly accomplished using quantitative polymerase chain reaction. Although various epigenetic regulations present insight into the possible biomarkers for diseases, the goal of using epigenetics to develop a stable diagnostic marker remains alluring. Despite clinical biomarkers, the development of precise epigenetic medicines as treatments for autoimmune skin disorders remains constrained. Striving to transform these epigenetic alterations into therapeutic therapies is worthwhile, notwithstanding the challenges in reaching the goal.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.