Influenza Vaccination Recommendations Save
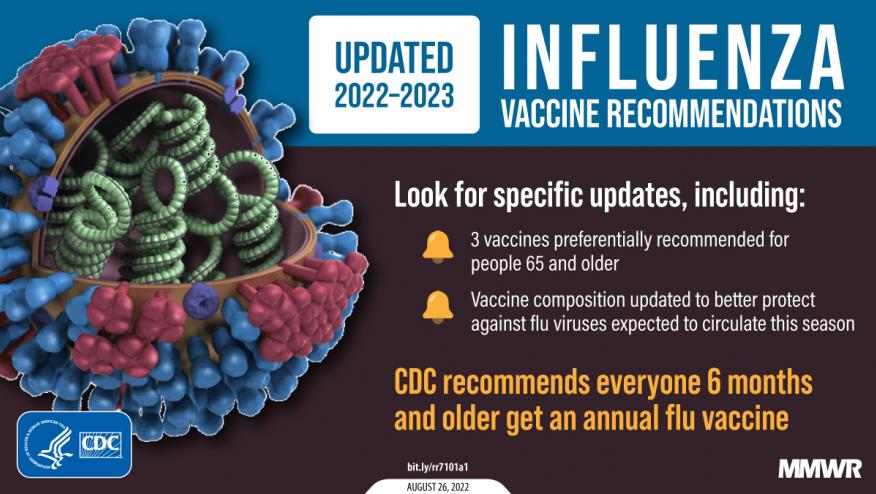
The CDC has published an update to the recommendations from the Advisory Committee on Immunization Practices (ACIP) on the use of seasonal influenza vaccines in the United States for the 2022-23 season.
Influenza viruses typically circulate annually in the United States, most commonly from the late fall through the early spring. Most persons who become ill after influenza virus infection recover without serious complications or sequelae. However, influenza can be associated with serious illnesses, hospitalizations, and deaths, particularly among older adults, very young children, pregnant persons, and persons of all ages with certain chronic medical conditions.
Routine annual influenza vaccination is recommended for all persons aged ≥6 months who do not have contraindications.
ACIP makes no preferential recommendation for a specific influenza vaccine, but notes preferences with the elderly (adults aged ≥65 years).
For the 2022–23 season vaccines are quadrivalent, inactivated influenza vaccines (IIV4s) or recombinant influenza vaccine (RIV4). A live attenuated influenza vaccine (LAIV4) is expected to be available. (Trivalent influenza vaccines are no longer available)
Influenza vaccines should be or soon to be available (after August 2022) and should be offered during September or October of 2022. Vaccination should remain available after October and throughout the season as long as influenza viruses are circulating.
ACIP recommends that adults aged ≥65 years preferentially receive any one of the following higher dose or adjuvanted influenza vaccines:
- quadrivalent high-dose inactivated influenza vaccine (HD-IIV4)
- quadrivalent recombinant influenza vaccine (RIV4)
- quadrivalent adjuvanted inactivated influenza vaccine (aIIV4)
Special Populations
- For most adults (particularly adults aged ≥65 years) and for pregnant persons in the first or second trimester: Vaccination during July and August should be avoided unless there is concern that vaccination later in the season might not be possible.
- Children who require 2 doses: Certain children aged 6 months through 8 years require 2 doses of influenza vaccine for the season (see Children Aged 6 Months Through 8 Years: Number of Influenza Vaccine Doses) (Figure). These children should receive their first dose as soon as possible (including during July and August, if vaccine is available) to allow the second dose (which must be administered ≥4 weeks later) to be received, ideally, by the end of October.
- Children who require only 1 dose: Vaccination during July and August can be considered for children of any age who need only 1 dose of influenza vaccine for the season. While waning of immunity after vaccination over the course of the season has been observed among all age groups (19–32), there are fewer published studies reporting results specifically among children (19–22). Moreover, children in this group might visit health care providers during the late summer months for medical examinations before the start of school. Vaccination can be considered at this time because it represents a vaccination opportunity.
- Pregnant persons in the third trimester: Vaccination during July and August can be considered for pregnant persons who are in the third trimester because vaccination might reduce risk for influenza illness in their infants during the first months after birth, when they are too young to receive influenza vaccine (33–36). For pregnant persons in the first or second trimester during July and August, waiting to vaccinate until September or October is preferable, unless there is concern that later vaccination might not be possible.
Vaccination provides important protection from influenza illness and its potential complications. During each of the six influenza seasons from 2010–11 through 2015–16, influenza vaccination prevented an estimated 1.6–6.7 million illnesses, 790,000–3.1 million outpatient medical visits, 39,000–87,000 hospitalizations, and 3,000–10,000 respiratory and circulatory deaths each season in the United States.
During the severe 2017–18 season, notable for an unusually long duration of widespread high influenza activity throughout the United States and higher rates of outpatient visits and hospitalizations compared with recent seasons, vaccination prevented an estimated 7.1 million illnesses, 3.7 million medical visits, 109,000 hospitalizations, and 8,000 deaths (14), despite an overall estimated vaccine effectiveness of 38% (62% against influenza A[H1N1]pdm09 viruses, 22% against influenza A[H3N2] viruses, and 50% against influenza B viruses).
During the pandemc, influenza circulated at historically low levels in the United States and globally during the 2020–21 influenza season. This was coincident with widespread implementation of nonpharmaceutical interventions (e.g., masking, social distancing, and suspension of in-person work and school) intended to prevent transmission of SARS-CoV-2 (the virus that causes COVID-19). Influenza activity increased during the 2021–22 season, although severity indicators (e.g., influenza-associated hospitalizations and deaths) were overall lower than in recent previous seasons.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.