Juvenile Idiopathic Arthritis - NEJM Review Save

Sandborg et al. has published an overview of juvenile idiopathic arthritis (JIA) - its classification, biology, genetics, , clinical presentations and treatment advances in the New England Journal of Medicine (NEJM).
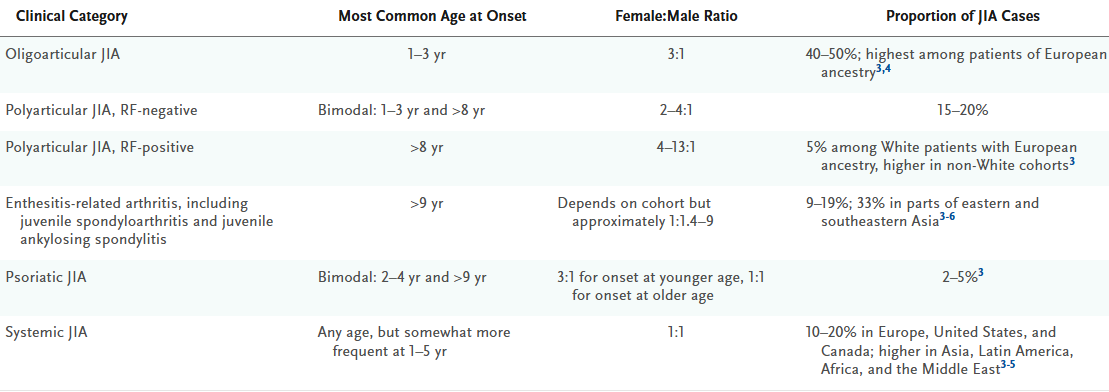
JIA is the most common form of inflammatory arthritis in the pediatric population and includes well characterized subtypes: oligoarticular JIA, polyarticular JIA, systemic JIA, psoriatic JIA, and enthesitis-related arthritis.
Prior to 2000 25-40% of JIA children ended up with moderate-to-severe disease, and lifelong complications. But the advent of newer antiinflammatory, biologic disease-modifying antirheumatic drugs (DMARDs) has substantially changed the management, and outcomes in JIA.
Highlights from this excellent overview include:
Classification: there are at least 5 major subtypes of JIA
- There is no definitive diagnostic tests for JIA - thus mimics need to be considered, including cancer, infections, and other autoimmune or autoinflammatory diseases
- Hallmark complications of JIA: asymptomatic chronic anterior uveitis, skeletal deformities (including deformity of the temporomandibular joint & micrognathia) .
- Oligoarticular JIA: has four or less joints at the onset, usually affecting girls between 1 and 5 years, many will have positive ANA tests. Half present with monoarthritis (knee usually). Approximately half may progress to a polyarticular course after 6 months. 30% may develop chronic anterior uveitis.
- Polyarticular JIA - may be seronegative or seropositive for RF. 15 to 20% of JIA cases are seronegative. Peak onset is between 1 and 3 years of age and again after 8 years. These patients may have a relapsing or chronic course. Seropositive Polyarticular JIA accounts for 5% of JIA cases with onset usually befor 9 years of age. They may be seropositive for RF, ACP and ANA as well. This group behaves like adult seropositive RA and may have an aggressive and destructive course and thus needs aggressive DMARD and biologic interventions.
- Enthesitis-Related Arthritis: Enthesitis and synovitis of peripheral joints (often lower extremities) is the presenting hallmark features. ERA includes those previously labeled as juvenile spondyloarthritis and juvenile ankylosing spondylitis. It affects boys more than girls and is uncommon before the age of 6 years. Symptomatic sacroiliitis, inflammatory spine disease develops in 40 to 60% usually during adolescence. Many will be HLA-B27+.
- Psoriatic JIA: peak incidence is at 2 to 4 years and after the age of 10 years (appears as a ERA subset). These appear as early-onset oligoarticular or rheumatoid factor–negative polyarticular JIA, usually female, with ANA positivity, and a risk of chronic anterior uveitis. Cutaneous psoriasis occurs in half but in many, the oligoarthritis predates the psoriais that may not develop until later in the disease. The PsA diagnosis may be supported by findings of dactylitis, nail pits or a family history of psoriasis. HLA-B27 is present in 10-12% of patients
- Systemic JIA (Still's disease): may occur at any age and accounts for 10-20% of all JIA patients. In addition to an onset of polyarthritis, sJIA is characterized by the acute onset of systemic inflammatory features such as inflammatory labs (ESR, CRP, Ferritin), quotidian fevers, evanescent rashes lymphadenopathy, hepatosplenomegaly, and serositis. In some arthritis may not be initially present. sJIA patients have a significant risk for life-threatening macrophage activation syndrome (MAS).
Refer to the article for discussion of specific therapies for these subsets, risk of complications (uveitis, skeletal abnormalities, MAS, lung disease)










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.