The Patient Journey with Rheumatic Disease Save

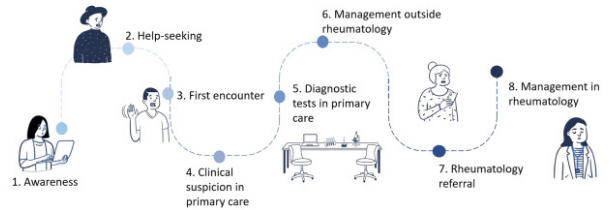
Oton and colleagues have reviewed the "patient journey" - from symptoms to specialty referral in those diagnosed with rheumatic and musculoskeletal diseases (RMDs). They identify the eight stages along the way and where improvements are needed.
This systematic review evaluated the quality of the literature to identify the delays, barriers or challenges in the RMD patient journey.
From a total of 27 studies (high or medium-high quality) they identified Eight touchpoints or phases for the patient journey:
- awareness
- help-seeking
- first encounter
- clinical suspicion in primary care
- diagnostic tests in primary care
- management (outside of rheumatology)
- rheumatology referral and
- management in rheumatology
Delays in diagnosis and treatment of RMDs are common and are associated with worse outcomes, increased suffering, and higher healthcare resource utilization.
This review highlights that RMD patient journeys are marked by frequent, fragmented barriers - such as limited disease awareness, normalization of symptoms, poor care coordination, and lack of streamlined referral pathways; and the need for enhanced education for healthcare providers, and a more patient-centred approach to management.
Highlights from this outstanding review, include:
- In 2020, 1.63 billion have RMDs, the second cause of nonfatal disability (projected to increase)
- Global burden of RMDs and their risk factors accounted for over 322 million new cases in 2019, 117 thousand deaths and 150 million disability-adjusted life-years (DALYs).
- Peak age for onset and DALYs of RMDs is 50-54 years, higher in women than in men
- Despite the prevalence and impact of RMDs, HCPs, PCPs and the public have limited awareness of RMDs
- Diagnostic delays are common - approximately 12 months for RA or 3-6 years for spondylarthritis (SpA) and fibromyalgia (FM), respectively
- RMDs are plagued by multimorbidity and polypharmacy, especially in the elderly
This review is a blueprint for effective interventions needed in the care of RMD patients and underscores that the problems are more than patient or primary care education about musculoskeletal diseases.
ADD THE FIRST COMMENT
Disclosures
The author has no conflicts of interest to disclose related to this subject










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.