Phase III Trials Back Bimekizumab for Spondyloarthritis Save
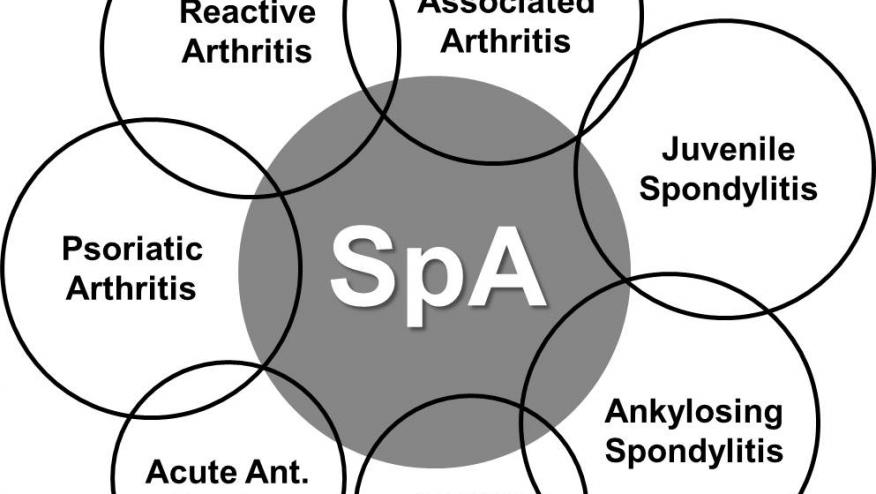
Bimekizumab, an investigational biologic drug targeting interleukin (IL)-17A/F, appeared highly effective in patients with axial spondyloarthritis (axSpA), researchers said.
With nearly 600 patients enrolled in two parallel phase III trials, 45% and 48% of those randomized to the active drug achieved at least 40% improvement in Assessment of SpondyloArthritis International Society ratings (ASAS40, the primary endpoint in both studies), compared with 21% and 23% of patients assigned to placebo (both P<0.001), according to Désirée van der Heijde, MD, PhD, of Leiden University in the Netherlands, and colleagues.
Secondary efficacy endpoints also strongly favored bimekizumab, the group reported in Annals of the Rheumatic Diseasesopens in a new tab or window.
Although adverse events, especially infections, were more common with the active agent, van der Heijde and colleagues called it "well tolerated" with no surprises relative to previous studies.
Bimekizumab was first tested in psoriasis, for which it is already approved in Europe and some other markets; a U.S. marketing application was rejected early last year after FDA inspectors raised questions about the drug's production. It's now reportedly on track for U.S. approvalopens in a new tab or window for psoriasis later this year. Bimekizumab has also completed late-stage studies in hidradenitis suppurativa.
Bimekizumab is unique in targeting the two IL-17 subspecies designated A and F. These are "key mediators of inflammation," van der Heijde's group explained. It therefore differs from biologics that inhibit IL-17A only, such as secukinumab (Cosentyx), and is hoped to be more effective as a result.
The two axSpA studies, dubbed BE MOBILE 1opens in a new tab or window and BE MOBILE 2opens in a new tab or window, enrolled patients with clinical axSpA (i.e., lacking clear imaging evidence of the disease) and radiographic axSpA, respectively. Participants were randomized 1:1 in BE MOBILE 1 and 2:1 in BE MOBILE 2 to the active drug or placebo, without other background medications. Bimekizumab was administered by injection every 4 weeks. Treatment lasted 16 weeks, at which point patients were evaluated for the primary and secondary endpoints. An 8-week, open-label extension then followed, during which the bimekizumab groups continued as before and the placebo groups were switched to the active drug.
Mean patient age was about 40, with a predominance of men in the studies. Roughly one in seven had previously used tumor necrosis factor (TNF) inhibitors. Disease activity ratings at baseline averaged 3.7 on the Ankylosing Spondylitis Disease Activity Score (ASDAS) and approximately 6.6 on the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI).
At week 16, BASDAI scores fell by an average of about 3 points with bimekizumab in both studies, while the placebo groups saw mean decreases of 1.5 and 1.9 points (both P<0.001). "Major improvement" in ASDAS scores were seen in about one-quarter of the bimekizumab groups, versus 5%-7% of those on placebo. Other efficacy measures, such as nocturnal spine pain and overall health status, gave similar results. Responses did not differ markedly by previous use of anti-TNF drugs.
During the 8-week extension, patients in the original placebo group showed improvements similar to those achieved during the main study with bimekizumab. The original active-drug group, meanwhile, had slight further improvements: for example, ASAS40 rates reached 52%-54% at week 24, while BASDAI scores fell another few tenths of a point on average.
Adverse event rates were similar between the placebo and bimekizumab groups, although they seemed bit higher in the patients with radiographic axSpA. The most common events that occurred more frequently with the active drug were nasopharyngitis (26-31% of patients receiving bimekizumab vs 12-16% on placebo during the primary 16-week phase), diarrhea (8-11% vs 3-5%), and oral candidiasis (3-4% vs 0%).
Fungal infections in general were an issue, occurring in 20%-23% of the bimekizumab groups versus none in the placebo groups. None were systemic, however. A few patients receiving bimekizumab experienced neutropenia (not seen with placebo), and rates of hepatic events were also somewhat higher with the drug.
A concern going into the trials was the possibility that bimekizumab could provoke new-onset inflammatory bowel disease, but this occurred in only three patients across the two trials, one of whom was taking placebo.
Summarizing the results, van der Heijde and colleagues wrote that bimekizumab "may therefore offer patients with axSpA an effective treatment option with a novel mode of action."









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.