RA Prevention through Deep Immunophenotyping Save
Researchers at the University of Colorado have identified pathogenic immune phenotypes in at-risk populations for rheumatoid arthritis (RA). They have found the expansion of specific T cell subtypes, in the at-risk group, and postulate this could lead to future immunospecific prevention strategies.
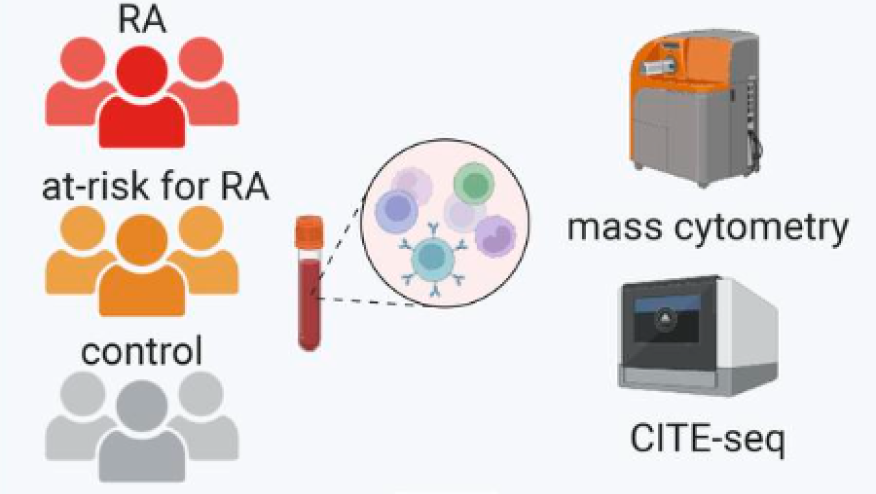
They applied multimodal single-cell technologies (mass cytometry and CITE-Seq) to characterize the immunophenotypes in whole blood from at-risk individuals (ARIs). Patients under study were chosen for either having citrullinated protein antibodies (ACPAs) and/or being first-degree relatives (FDR) of an RA patients. Findings were compared to either established RA or healthy control groups.
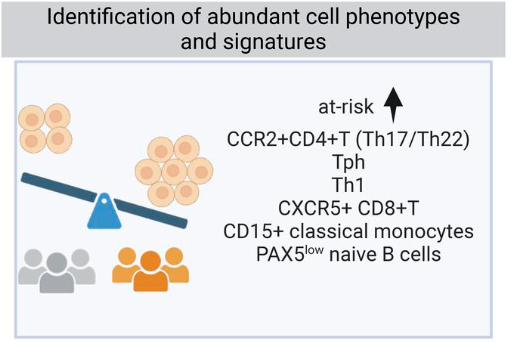
ARIs they found expansion of CCR2+CD4+ T cells, T peripheral helper (Tph) cells, type 1 T helper cells, and CXCR5+CD8+ T cells.
- In ACPA-negative FDRs: CD15+ monocytes were expanded
- In ACPA- positive FDRs: activated PAX5lo naive B cell population was expanded
- CCR2+CD4+ T cells expressedhigh levels of Th17- and Th22-related transcripts (including CCR6, IL23R, KLRB1, CD96, and IL22)
Zhang et al. will apply these tools to complex datasets to subjects enrolled in the preclinical trial called StopRA that showed no effect of hydroxychloroquine as a preventative intervention. They will examine the immunophenotypes of people who progressed to RA, versus those who didn’t.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.