BSR Guidelines for Giant Cell Arteritis Save
NICE has commissioned an update to the 2010 British Society for Rheumatology (BSR) guideline for the management of giant cell arteritis (GCA), and proposed a total of 19 recommendations for the diagnosis and treatment of GCA.
These guidelines were needed since GCA should be considered a medical emergency, and may be diagnosed and treated by clinicians in primary and specialez care with a wide variety of clinical backgrounds.
The objective was to provide up to date recommendations based on recent evidence and when evidence was not fully available, based on expert consensus and consideration of current practices. This guideline excluded recommendations for Takayasu's arteritis and polymyalgia rheumatica.
General Principles
- Patients in whom GCA is strongly suspected should be immediately treated with high-dose glucocorticoids. Consensus score: 9.61.
- GCA is a medical emergency. Each local healthcare organization should have information available to front-line clinicians, such as general practitioners and clinicians working in acute care, on how to refer patients with suspected GCA urgently for local specialist evaluation. Patients should be evaluated by a specialist ideally on the same working day if possible and in all cases within 3 working days. Consensus score: 9.17.
- Patients with suspected GCA should be evaluated by a clinician with appropriate specialist expertise, usually a rheumatologist. Patients presenting with a history of new visual loss (transient or permanent) or double vision should be evaluated as soon as possible on the same calendar day by an ophthalmologist. Consensus score: 9.61.
- When starting glucocorticoids for suspected GCA, diagnostically relevant symptoms and signs should be documented. Blood should be taken for full blood count, CRP and ESR before or immediately after commencing high-dose glucocorticoids. If GCA is strongly suspected, the first dose of glucocorticoid can be given without waiting for laboratory results. Consensus score: 9.61.
- Patients treated for GCA should be evaluated for features of the disease relevant to the prognosis, such as clinical and laboratory features of a marked inflammatory response at diagnosis, ischaemic manifestations such as transient visual loss or jaw/tongue claudication and signs or symptoms indicating involvement of the aorta and its proximal branches, and for comorbidities relevant to treatment, such as diabetes mellitus, hypertension and bone fracture risk. Consensus score: 9.53.
- Full assessment of the disease and comorbidities and consideration of the patient’s personal priorities should inform decisions about glucocorticoid tapering and initiation of additional treatments such as glucocorticoid-sparing therapies. Involvement of and clear communication with primary care physicians is critical, especially for management of multimorbidity. Consensus score: 9.67.
- All patients with GCA should be provided with information about GCA and its treatment. Patients should receive advice on diet, physical activity and stopping smoking. Consensus score: 9.47.
- During glucocorticoid taper and after glucocorticoid cessation, patients should be informed what symptoms may suggest GCA relapse and what action the patient should take in these circumstances, including the first point of contact for medical advice and how to contact the team providing specialist care. Consensus score: 9.81.
Specific Recommendations on Diagnostic Testing
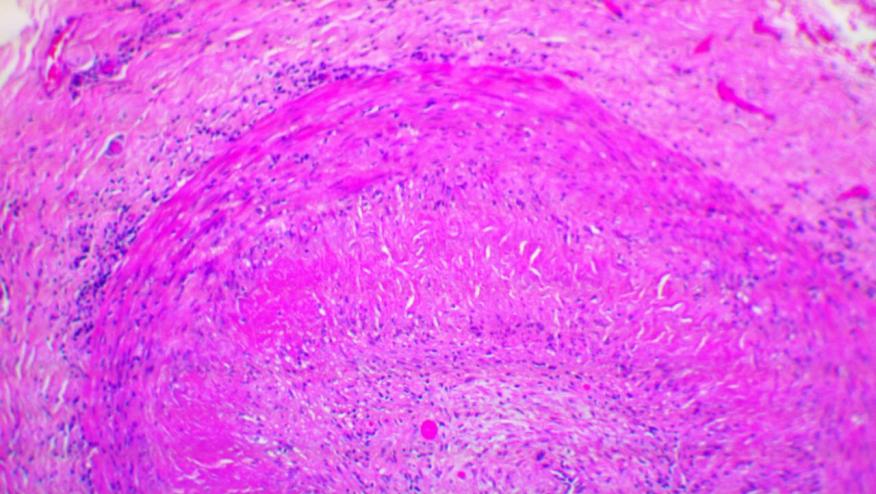
- Strong recommendation: Patients with suspected GCA should have a confirmatory diagnostic test. This could be either a temporal artery biopsy at least 1 cm in length or an ultrasound of the temporal and axillary arteries, or both. QoE: +++. Consensus score: 9.33
- Conditional recommendation: 18F-FDG-PET, MRA, CTA or axillary artery ultrasound may be used to evaluate involvement of the aorta and its proximal branches. QoE: +. Consensus score: 9.36
Recommendations on Treatment of GCA
- Conditional recommendation: The standard initial glucocorticoid dose for GCA is 40–60 mg oral prednis(ol)one per day. QoE: +. Consensus score: 9.44.
- Conditional recommendation: GCA patients with acute or intermittent visual loss may initially be given 500 mg–1 g intravenous methylprednisolone daily for up to 3 consecutive days before commencing oral prednis(ol)one therapy. If intravenous therapy is not immediately possible, this should not delay initiation of oral prednis(ol)one. QoE: +. Consensus score: 9.00.
- Conditional recommendation: Glucocorticoid dose should be tapered to zero over 12–18 months, providing there is no return of GCA symptoms, signs or laboratory markers of inflammation. A more rapid dose reduction is appropriate for patients at high risk of glucocorticoid toxicity and/or those receiving concomitant glucocorticoid-sparing therapy. QoE: +. Consensus score: 8.81.
- Conditional recommendation: Patients should be prescribed a single daily dose of glucocorticoid rather than alternate day dosing or divided daily dosing. QoE: +. Consensus score: 9.53
- No recommendation can be made for the use of modified-release prednisone in the treatment of GCA. QoE: insufficient evidence. Consensus score: 9.72.
- Conditional recommendation: MTX might be considered for GCA, in combination with a glucocorticoid taper, in patients at high risk of glucocorticoid toxicity or who relapse. There is insufficient evidence to recommend any other oral immunosuppressive agent in GCA, including azathioprine, leflunomide or mycophenolate mofetil. QoE: ++. Consensus score: 8.92.
- Strong recommendation: Tocilizumab can be considered for GCA, in combination with a glucocorticoid taper, especially in patients at high risk of glucocorticoid toxicity or who relapse. TNF inhibitors are not recommended in GCA. QoE: +++. Consensus score: 9.61.
- The routine use of antiplatelet or anticoagulant agents for GCA is not recommended. QoE: insufficient evidence. Consensus score: 9.28.
- The routine use of cholesterol-lowering agents such as statins for GCA is not recommended. QoE: insufficient evidence. Consensus score: 9.53.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.