Clinical Associations with Myositis Antibodies Save

While myositis-specific autoantibodies (MSAs) and myositis-associated autoantibodies (MAAs) may have prognostic value through their clinical associations, many patients will not have them and overall, they are poorly predictive of a malignancy risk.
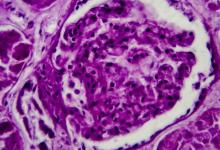
A single center analysis of 51 polymyositis (PM) and 36 dermatomyositis (DM) patients assessed clinical associations and autoantibodies by immunoblot assays. The MSAs included anti-Jo-1, anti-PL-7, anti-PL-12, anti-EJ, anti-OJ, anti-SRP, anti-Mi-2α, anti-Mi-2β, anti-TIF-1γ, anti-MDA5, anti-NXP-2, and anti-SAE1. The MAAs included anti-PM-Scl 75, anti-PM-Scl 100, anti-Ku, anti-SSB/La, anti-SSA/Ro, and anti-Ro-52 kDa.
Nearly 70% of patients were women. MSAs were found in 72% of patients and MAAs were observed in 49%. MSAs coexisted with MAAs in 35.6% of cases. The most common coexisting antibody was anti-Ro-52, found in 11 patients (2/3) with anti-Jo-1 antibodies.
Clinical associations
- Interstitial lung disease (ILD) was seen in two-thirds of PM patients, most associated with anti-Jo-1 or anti-PL-12 antibodies
- Patients anti-MDA5 antibodies - 7/8 had an amyopathic form, and more frequent ILD, skin changes and arthralgias
- anti-SRP was strongly associated with the Raynaud's phenomenon and the highest muscle enzyme levels
- Malignancy was found in 16% of patients (equally common in PM and DM)
- anti-TIF-1γ was most common Ab related to cancer
- anti-Mi-2α (in both DM and PM) was typically accompanied by skin changes, but not ILD
While MSAs and MAAs may help to predict the clinical course of the autoimmune myopathy, they were absent in 30% of typical PM or DM cases.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.