ICYMI: COVID-19 and Thrombotic Complications Save
Editor's note: This article was originally published May 7, 2020 and is being shared again this week in case you missed it.
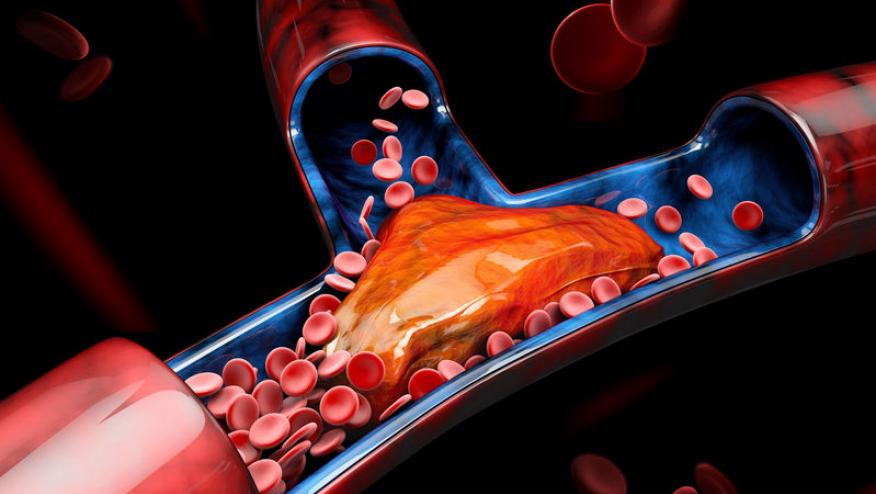
Severe and fatal outcomes with coronavirus infection are often the result of the downstream damage that follows the viral infection. Rising high on the list of complications are the hematologic and vascular complications seen in severely affected patients, so much so that many centers are routinely anticoagulating hospitalized (but not ambulatory) COVID patients.
Vascular pathology is evident on post mortem studies of the lungs. A recent report of 21 autopsies showed "exudative diffuse alveolar damage with massive capillary congestion often accompanied by microthrombi despite anticoagulation". Ten had superimposed bronchopneumonia, but there was also evidence of pulmonary embolisms (n=4), alveolar haemorrhage (n=3), vasculitis (n=1) and generalised thrombotic microangiopathy (3). Many of these fatal cases also had comorbidities (hypertension, obesity, cardiovascular diseases) known to portend poor outcomes in COVID infection (1).
A new article by Gavriilaki and Brodsky reviewed the thrombotic microangiopathy (TMA) associated with COVID, noting the TMA appears to be more a complement-mediated thrombotic micoangiopathy, rather than that due to sepsis-induced coagulopathy or disseminated intravascular coagulation (DIC)(2). Complement TMA characteristically has microangiopathic hemolytic anemia, thrombocytopenia, organ damage (CNS, renal, cardiac), anemia, thrombocytopenia and high LDH; features similar the catastrophic antiphospholipid syndrome (CAPS). It is presumed that organ damage is at least, partly from microvascular thrombosis.
Coronaviruses have been shown to activate complement via the lectin pathway and there is evidence of complement-mediated inflammatory lung damage with complement deposits in lung and skin biopsies. Whether COVID can give rise to a complementopathy that incites TMA or CAPS needs further study. There are 2 FDA approved therapies (for PNH) to inhibit complement activation, eculizumab and ravulizumab, both binding to C5 to inhibit downstream complement activation. This approach is currently under study in COVID-19.
Today there is a NEJM letter on lupus anticoagulant (LAC) activity in COVID patients (3). They describe 216 patients with severe acute respiratory coronavirus 2 (SARS-CoV-2) in whom 44 (20%) had a prolonged aPTT. Only 2 patients had venous thromboses (1 PE) and ther were no arterial thromboses or bleeding. Further assays on 34 patients found 31 (91%) who were LAC positive. They found that LAC were significantly higher among in Covid-19 patients than in a comparator control cohort (P<0.001). While the role of LAC in COVID merits further study, they suggest that a prolonged aPTT should not deter the use of anticoagulation therapies in the prevention or treatment of venous thrombosis in COVID-10 patients.
Another report in the NEJM described three COVID infected patients, who developed peripheral and central infarcts with IgA anticardiolipin antibodies as well as anti–β2-glycoprotein I IgA and IgG antibodies.
Thus, it appears vasculopathy, possibly complement and/or autoantibody mediated, may be one of several final damage pathways in severe COVID-19 patients. Currently, anticoagulation is standard in such patients, while we await the clinical trial results utilizing complement inhibitors (eculizumab).
References
1. Menter T, et al. Histopathology. 2020 May 4.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.