Post-Menopausal Osteoporosis Review and Recommendations Save
A recent New England Journal review of post-menopausal osteoporosis (OP) provided updated information, strategies and a review of guidelines and clinical recommendations.
Salient highlights from this review include:
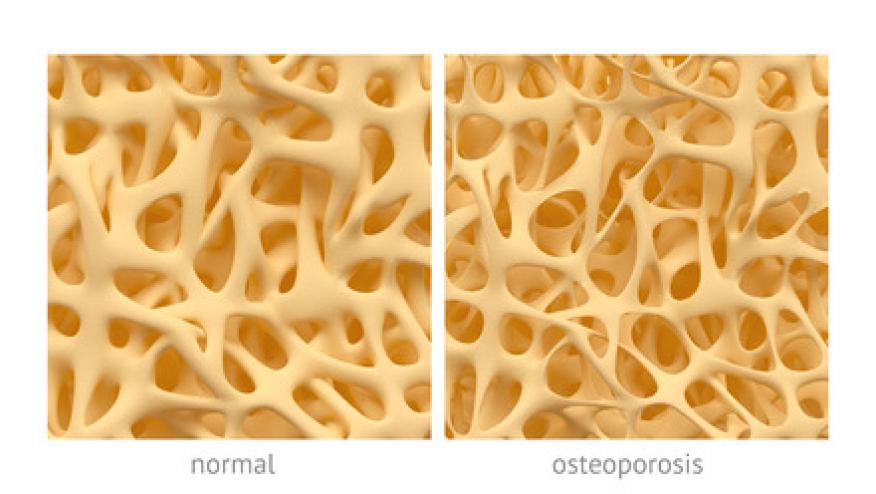
- Postmenopausal osteoporosis is defined as the occurrence of a fragility fracture (with no associated trauma or with minimal trauma equivalent to falling from a standing height or less) or a bone mineral density (BMD) at the spine, total hip, or femoral neck that is at least 2.5 standard deviations below the mean (T score of −2.5 or less)
- In the USA, nearly 20% of women over 50 years of age and 30% of women >65 years of age have osteoporosis.
- 40% of postmenopausal women have low bone mass (osteopenia)
- ~ 50% of postmenopausal women will have fragility fractures: with pain, disability, and decreased quality of life.
- Following a hip fracture, many women never regain independence, 20% are institutionalized, and the risk of death within 1 year doubles.
- Non-White women who have hip fractures are more likely to die within 6 months
- The health care cost associated with postmenopausal OP fractures is estimated to be $57 billion annually, iand s projected to exceed $95 billion by 2040.
-
Treatment of postmenopausal osteoporosis is recommended for:
-
Any OP fragility fracture (regardless of the BMD);
-
T score of −2.5 or less at the lumbar spine, total hip, or femoral neck;
-
High 10-year fracture risk according to FRAX or a hip fracture risk of ≥3% or major osteoporotic fracture risk of ≥20%
-
-
FDA-approved treatments are based on T scores or fracture criteria (or both). Evidence supporting treatment based on FRAX-estimated fracture risk is less robust
-
OP risk stratification should be based on the T score, presence of fractures, and FRAX score (to determine if at “high risk” or “very high risk.”)
-
Lifestyle changes should include:
-
Stop smoking, avoid excessive alcohol, increase weight-bearing exercise, and prevent falls
-
1000 to 1200 mg of calcium daily
-
400 to 1000 IU of vitamin D daily (Some recommend adjusting vitamin D intake to achieve serum 25-hydroxyvitamin D levels higher than 20 to 30 ng per milliliter, but this is not backed by strong data)
-










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.