Prevalence of Arthritis Rising in the USA Save

The latest CDC estimates of the national prevalence of arthritis and arthritis-attributable activity limitations (AAAL) show a continued increase in absolute number: 58.5 million (23.7%) U.S. adults have arthritis, 25.7 million (43.9%) of whom have AAAL.
Arthritis has been the most frequently reported main cause of disability among U.S. adults for >15 years (1), was responsible for >$300 billion in arthritis-attributable direct and indirect annual costs in the U.S. during 2013 (2), is linked to disproportionately high levels of anxiety and depression (3), and is projected to increase 49% in prevalence from 2010-2012 to 2040 (4).
To update national prevalence estimates for arthritis and arthritis-attributable activity limitation (AAAL) among U.S. adults, CDC analyzed combined National Health Interview Survey (NHIS) data from 2016–2018. An estimated 58.5 million adults aged ≥18 years (23.7%) reported arthritis; 25.7 million (10.4% overall; 43.9% among those with arthritis) reported AAAL. Prevalence of both arthritis and AAAL was highest among adults with physical limitations, few economic opportunities, and poor overall health. Arthritis was reported by more than one half of respondents aged ≥65 years (50.4%), adults who were unable to work or disabled* (52.3%), or adults with fair/poor self-rated health (51.2%), joint symptoms in the past 30 days (52.2%), activities of daily living (ADL)† disability (54.8%), or instrumental activities of daily living (IADL)§ disability (55.9%). More widespread dissemination of existing, evidence-based, community-delivered interventions, along with clinical coordination and attention to social determinants of health (e.g., improved social, economic, and mental health opportunities), can help reduce widespread arthritis prevalence and its adverse effects.
Using the NHIS (an ongoing, nationally representative, in-person interview health survey of the U.S. civilian population), arthritis was ascertained by a response of “yes” to, “Have you ever been told by a doctor or other health care professional that you have arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?” AAAL was ascertained among those with arthritis by a response of “yes” to, “Are you now limited in any way in any of your usual activities because of arthritis or joint symptoms?”
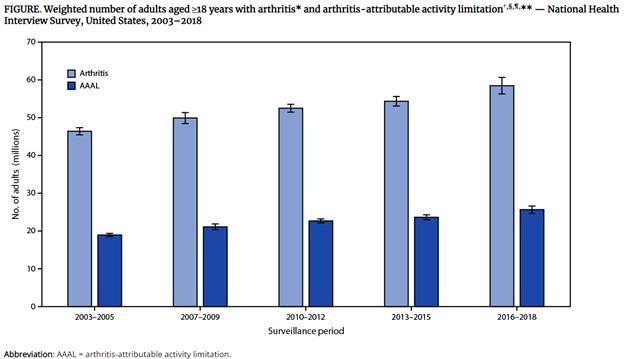
During 2016–2018, 58.5 million U.S. adults aged ≥18 years (23.7%; 21.5% age-standardized) are estimated to have arthritis; 25.7 million (43.9%; 40.8% age-standardized) of those with arthritis are estimated to have AAAL (Figure), representing 10.4% (9.4% age-standardized) of the total U.S. adult population.
Annualized absolute prevalence of both arthritis and AAAL continues nearly two decades of an increasing statistically significant linear trend (Figure).
Prevalence of arthritis increased with increasing age, body mass index (BMI), aerobic physical inactivity, and worsening psychological distress and self-rated health, and decreased with increasing educational attainment and income-to-poverty ratio (Table 1). Arthritis prevalence was >50% among adults aged ≥65 years (50.4%), adults who were unable to work or disabled (52.3%), and adults with fair/poor self-rated health (51.2%), joint symptoms in the past 30 days (52.2%), ADL disability (54.8%), and IADL disability (55.9%).
The unadjusted prevalence of AAAL exceeded 50% in several groups, including:
- Those with joint symptoms in the past 30 days (51.6%)
- Unable to work or disabled (54.7%)
- Adults of other/multiple races (54.5%)
- non-Hispanic American Indian or Alaska Natives (60.7%)
- Adults with low income (53.3%) or poor/near poor income-to-poverty ratios (63.3%)
- Moderate psychological distress (59.5%)
Annualized estimates from 2016–2018 indicate that the number of U.S. adults with arthritis (58.5 million) and AAAL (25.7 million) increased compared with 2013–2015 estimates (54.4 million and 23.7 million, respectively).
These increases could be attributable to population aging and other contributing factors (e.g., obesity) are expected to sustain these trends, public health, medical, and senior and other service systems face substantial challenges in addressing the needs of adults with arthritis, who already account for nearly one quarter of U.S. adults.
A coordinated approach of expanding intervention implementation among adults already limited by arthritis while mitigating future negative arthritis effects by creating “social, physical, and economic environments that promote attaining the full potential for health and well-being,” could help improve quality of life and limit the personal and societal impacts of arthritis.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.