Renal Involvement is Pivotal in ANCA-Associated Vasculitis Save
Bearing in mind that renal impairment is among the worst complications of ANCA-associated vasculitis (AAV), researchers have identified four different trajectories of kidney function over time in AAV patients, with implications for personalized treatment, as well as future research.
In a cohort of 225 patients, 20 experienced rapid decline, 82 showed stable impairment, 129 had stable near-normal function, and 24 showed increases in kidney function, reported Zachary S. Wallace, MD, MSc, of Massachusetts General Hospital in Boston, and colleagues.
Not surprisingly, perhaps, patients showing the worst renal outcomes tended to be those with the most comorbidities and relatively poor kidney function prior to developing vasculitis, they noted in Arthritis Care & Research.
The findings highlight "the importance of personalized, multidisciplinary care for AAV patients; further investigation of tailored strategies to preserve renal function is warranted," Wallace and colleagues concluded.
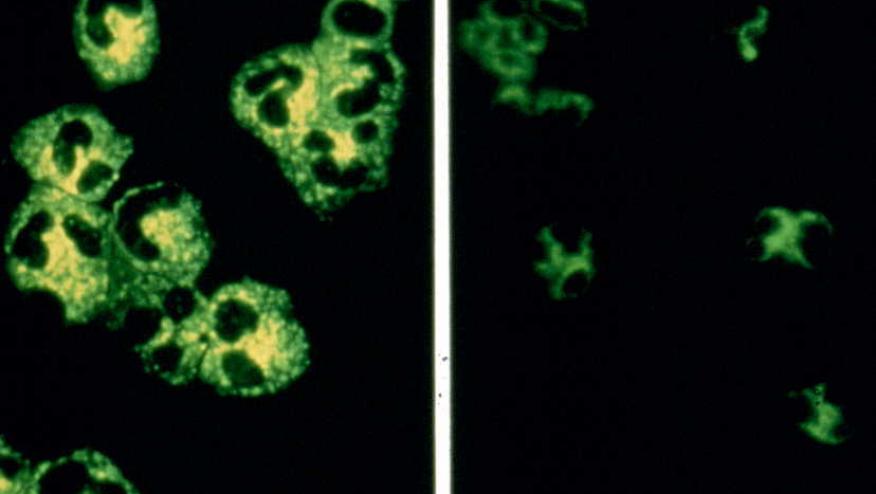
AAV is a closely related family of autoimmune conditions in which antibodies develop against neutrophils, leading not to their destruction but to overactivation. The result is inflammation and eventual destruction of small blood vessels. The kidneys, of course, are rich in small vessels, and thus renal complications affect more than half of AAV patients.
What isn't known, however, is how renal impairment develops and progresses over time in tandem with vasculitis. Wallace and colleagues pointed to an earlier study of AAV patientsopens in a new tab or window in whom nearly half of end-stage renal disease (ESRD) cases occurred "with no clinical evidence of active vasculitic renal disease at the time of ESRD onset."
"There has been little work using longitudinal data to characterize and differentiate slow progressors from those who experience rapid renal function deterioration early in their disease course," Wallace and colleagues wrote.
To take a closer look at this issue, the group examined records of 225 AAV patients treated at Mass General and its sister institution, Brigham and Women's Hospital, from 2002 to 2017. These patients had kidney function tests prior to starting AAV-specific therapy and continuing thereafter, with up to 10 years of follow-up. The key outcomes were change in estimated glomerular filtration rate (eGFR), over a period beginning 1 year before starting treatment and ending 2 years after, and time to onset of ESRD. (The latter was identified via chart codes for chronic dialysis or kidney transplant.)
All of the "rapid-decline" group developed ESRD, mostly by the time AAV treatment started. Prior to beginning treatment, their eGFR values averaged 48 mL/min/1.73 m2, declining essentially to zero during the first year of therapy. Notably, median Charlson Comorbidity Index score in this group was 4.5 (interquartile range 3.5-6), higher than in the other groups.
Pretreatment eGFR values were similar in the "stable impaired" group but showed no visible decline during follow-up: the pretreatment mean was 44 mL/min/1.73 m2 and stood at 48 at year 5 of follow-up. In the "stable normal" group, eGFR values hovered around 70 mL/min/1.73 m2 throughout follow-up. Only a few people in these two groups developed ESRD (7% each).
The fourth group was the oddest. Initially it resembled the rapid-decline group, with eGFR values plummeting during the year before starting treatment and for some months after. But at year 1 of treatment, mean eGFR had recovered somewhat, reaching 24 mL/min/1.73 m2 from a level of 10 at the start of therapy, and it continued to rise. By year 5, eGFR in this group averaged 58 mL/min/1.73 m2.
Wallace and colleagues had no firm explanations for the different trajectories. They did observe that the "stable impaired " group skewed older and with more comorbidities than the "stable normal" and "recovery" groups. While one could speculate that AAV therapy had helped reverse microvascular damage in the fourth "recovery" group, the researchers cautioned against attributing any of the renal trajectories to effects of treatment, "due to the likely role of confounding by indication."
"These observations highlight high-risk patients who might benefit from a personalized approach to care based on their age, comorbidity burden, and renal function trajectory," Wallace and colleagues wrote. "Indeed, even by three months, there were striking differences in the trajectory of renal function among those classified in the impaired versus recovery groups, highlighting the implications of persistent renal dysfunction at this time point."
Limitations to the study included the small number of patients, its single-center design, and reliance on administrative records.
Source Reference: Hanberg JS, et al "Longitudinal patterns of renal function in ANCA-associated vasculitis" Arthritis Care Res 2023; DOI: 10.1002/acr.25100.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.