Should Lupus Nephritis Receive PJP Prophylaxis? Save

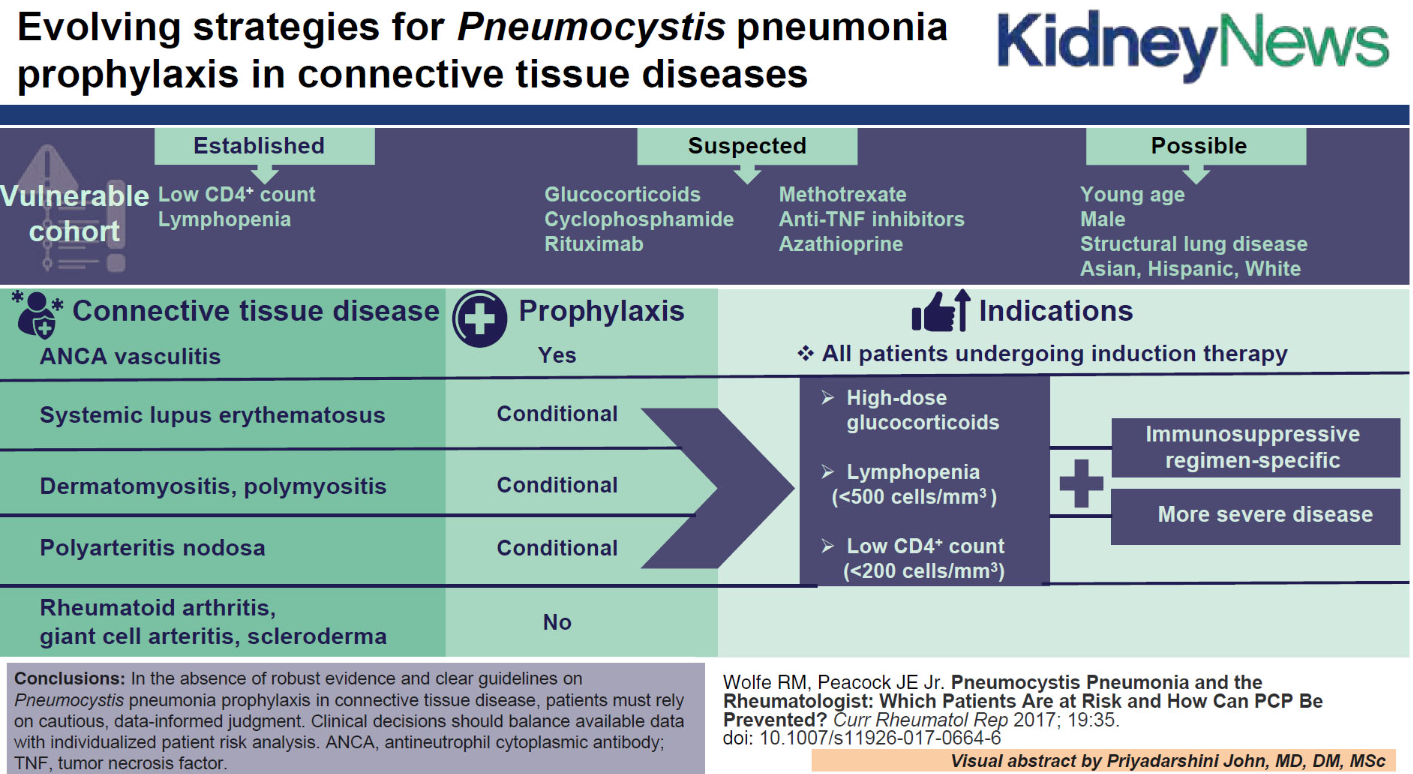
A current review article suggests that the need for Pneumocystis jirovecii pneumonia (PJP) prophylaxis in patients with systemic lupus erythematosus (SLE) and lupus nephritis will need to be individualized based on therapies and risk factors.
There are no clear guidelines for PJP prophylaxis in SLE and LN. But added use of immunosuppressive medications and systemic corticosteroids may change this consideration, especially since patients with autoimmune disease and PJP may have an estimated mortality of 40% to 50%.
A 2014 Cochrane Systematic Review "concluded that PJP prophylaxis is warranted when the risk of infection exceeds 6%, which corresponds to a number needed to treat (NNT) of approximately 20". Yet, the frequency of PJP varies greatly among autoimmune diseases, and the therapies employed.
SLE has a low risk of PJP infection, suggesting prophylaxis is not generally warranted. Moreover the use antibiotic prophylaxis (trimethoprim-sulfamethoxazole), is associated with more than 10% risk of side effects (rash, drug allergy, cytopenias, disease flares).
The review authors suggest a "more targeted or conditional approach" wherein one weights TMP/SMZ harms vs risk of PJP. Risk factors for PJP infection that may warrant prophylaxis include:
- low absolute lymphocyte count (no consensus exists yet on the exact threshold)
- low CD4+ count (<200 cells/mm3)
- presence of concomitant structural lung disease
With the new 2024 ACR guidelines for LN (class III/IV) calling for triple therapy (steroids, MMF, voclosporin or belimumab), PJP risk needs to be considered. Other known, and important risk factors for PJP include the use of high dose steroids and rituximab. There is no clear or certain risk of PJP with other forms of B cell depletion (Belimumab, CAR-T cell, etc).










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.