Extrapulmonary Manifestations of COVID-19 Save
A new article in Nature Medicine delineates how our understanding of COVID-19 infection has evolved over time, such that the infection outomes may be worsened by extrapulmonary manifestations; notably thrombotic, cardiac, renal, gastrointestinal hepatic, neurologic, and other complications.
Tissue damage may ensue whereever the SARS-CoV-2 virus gains entry via ACE2 receptor binding. While the lung may be the primary attack site, entry through the GI tract, spread to nodes and other tissues may lead to endothelial damage, thrombotic events and altered immune responses with hyperinflammation. The article lists several complications occuring outside of the lungs and COVID pneumonia.
Thrombotic complications
Thrombotic complications may occur with infection, but the COVID experience suggests a higher than expected rate of clotting and bleeding disorders. Presumeably this stems from virus associated endothelial damage leading to both big and small vessel thrombotic complications. Emerging research suggests a thrombotic microangiopathy (TMA) that is different from disseminated intravascular coagulation (DIC)(2). Moreover, ther are may reports of and patients with lupus anticoagulant (LAC) and antiphospholipid antibodies in those with organ damage affecting the brain, lungs, liver etc.
Hyperimmune consequences
A subset of those hospitalized with COVID-19 infection will escalate their problems with evidence of unregulated, hyperinflammation - some of which has been labeled cytokine storm syndrome (AKA macrophage activation syndrome). This is validated by the magnitude of proinflammatory markers and the favorable uncontrolled reports showing benefits to dexamethasone, IL-1 (eg, anakinra) and IL-6 (eg, tocilizumab) inhibition and colchicine. Fortunately there are many trials in progress further evaluating a plethora of immunomodulatory and antiinflammatory interventions.
Cardiac complications
Beyond a state of COVID-induced thrombotic potential there are several cardiac complications of COVID, including MI, myocarditis, cardiomyopathy, cor pulmonale, and Kawasaki-like disease affecting the hearts of children with COVID-19. While it is clear that patients with pre-existing cardiac disease and risk factors are at higher risk for cardiac complications and demise, there are those who have developed cardiac complications without pre-existing conditions.
Kidney complications
Acute kidney damage, proteinuria and hematuria are uncommonly seen in COVID-19 infection, with less than 10% of patients requiring dialysis.
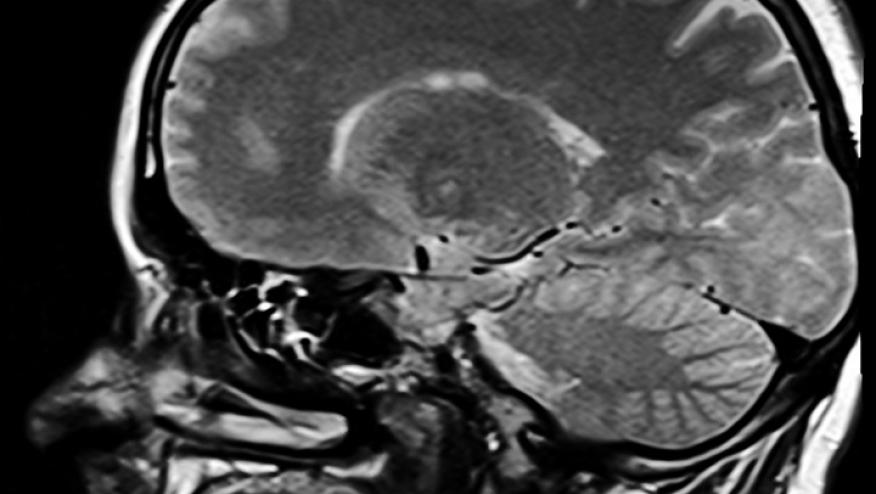
Neurological complications
Encephalopathy, ageusia, headache, CVA, dizziness, fatigue, delirium and hallucinations have been described.
Gastrointestinal complications
GI features are less prevalent but includes reports of anorexia, nausea and/or vomiting, diarrhea, and abdominal pain and very rarely gastrointestinal bleeding.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.