ICYMI: BSR Guideline on Management of Sjogren’s Syndrome Save
Editor's note: This article originally appeared April 16, 2024, and is being shared again while RheumNow enjoys the July 4th holiday. Enjoy!
Sjögren disease (SD) is the most common of all autoimmune disease, yet little is know of its etiology and there are insufficient interventions for those affected with mucosal or systemic manifestations.
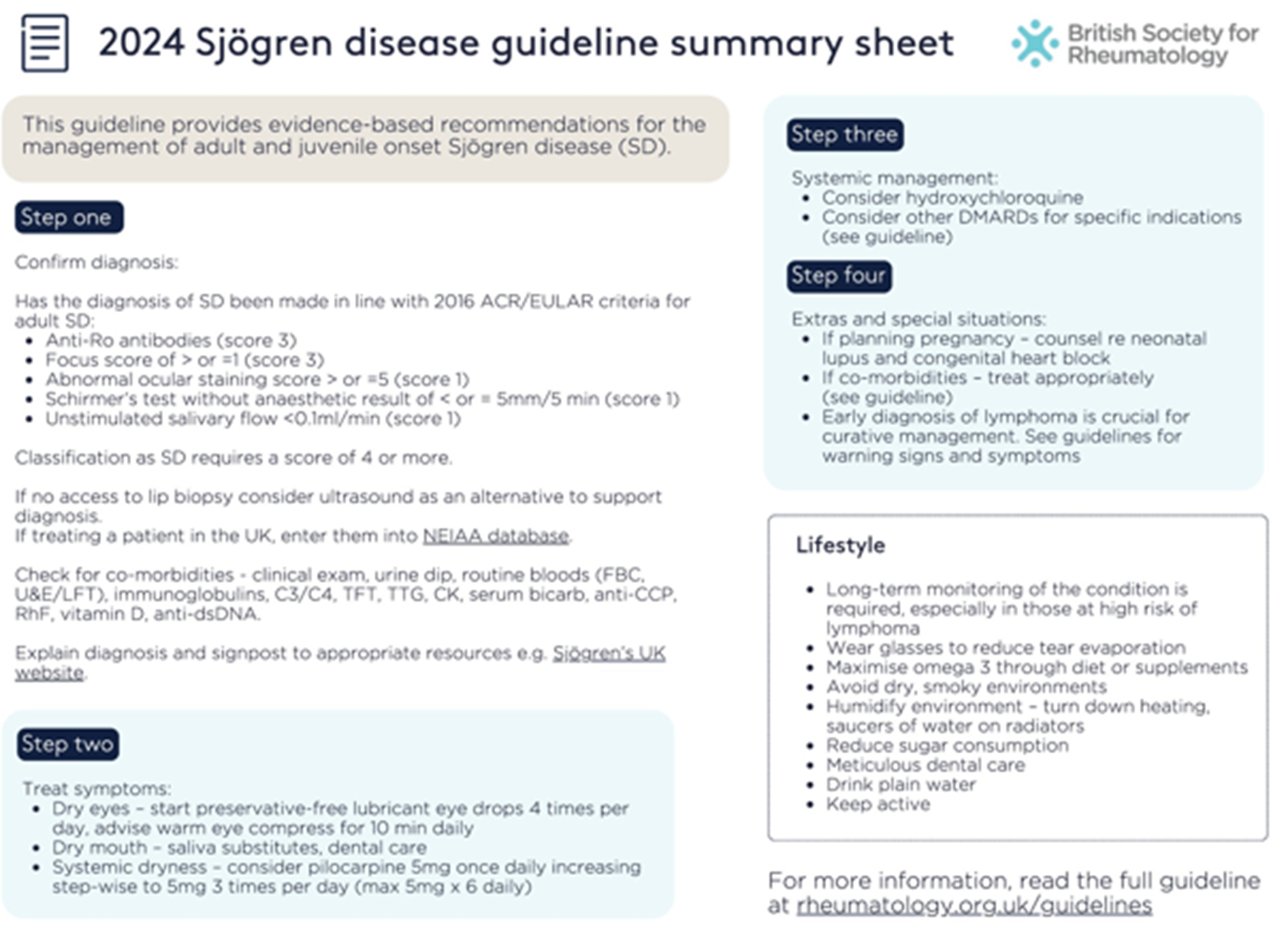
The British Society of Rheumatology has updated its 2017 guidelines, with wider evidence and recommendations for the management of children and adolescents with SD. This article reviews the data and recommendations stemming from 19 questions on SD care. An abbreviated version of these Questions and recommendations are provided below.
1. In people suspected of having SD, what is the diagnostic accuracy of ANA, ENA and other novel antigen testing?
- Do not measure ANA in the absence of clinical indicators of SD or other CTD (1, C) (SOA 94.6%).
- Use ANA as a screening antibody where there is clinical suspicion of a CTD (1, C) (SOA 93.9%).
- Measure ENA even if the ANA is negative if there is a high index of suspicion of SD (1, C) (SOA 96.7%).
2a. In people suspected of having SD, what is the diagnostic accuracy of salivary gland US scanning?
- USS of the salivary glands can provide useful additional information to support either the presence of or lack of evidence for SD (1, A) (SOA 95.2%).
- USS does not currently replace either antibody testing or histological analysis in adult SD classification criteria (1, A) (SOA 96.4%).
2b. In people suspected of having SD, what is the diagnostic accuracy of other imaging modalities?
- Overall, although they may provide useful supplementary information, we do not recommend additional imaging modalities over and above USS in the routine assessment of SD (1, C) (SOA 97.3%).
3a. In people suspected of having SD, what is the diagnostic accuracy of major and minor salivary gland biopsy?
- Consider a minor labial salivary gland biopsy to aid diagnosis in those with clinically suspected SD where the diagnosis cannot be made by clinical and serological features alone (1, A) (SOA 98.2%).
3b. In people suspected of having SD, what is the diagnostic accuracy of lacrimal gland biopsy?
- There is currently insufficient evidence to routinely recommend lacrimal gland biopsy in SD (1, C) (SOA 98.2%).
4a. In people with confirmed SD are there any measurable biomarkers that can predict development of lymphoma?
- Individuals with SD should be offered further investigation early if they present with new salivary gland swelling or other symptoms that might suggest the development of lymphoma (1, A) (SOA 98.75%).
- Consider a minor labial salivary gland biopsy to provide additional prognostic data regarding lymphoma risk in both seronegative and seropositive individuals (2, C) (SOA 92.7%).
4b. In people with confirmed SD are there any measurable biomarkers that can predict disease progression or development of extraglandular disease?
- Baseline assessment of individuals with SD should include a thorough clinical and serological evaluation to inform the risk of development of extraglandular features and disease progression (1, B) (SOA 97.6%).
5. In people with confirmed SD what other investigations should routinely be undertaken to exclude common associated conditions, for example coeliac or thyroid disease?
- Be aware of and consider screening for commonly associated conditions, as guided by age and/or clinical presentation (1, B) (SOA 94.7%).
- We recommend that the following additional investigations are undertaken at baseline, and repeated as clinically indicated, to detect comorbidities and associated autoimmune diseases:Vitamin D, Thyroid function, LFTs, TTG, Igs, SPEP, Serum bicarbonate, Creatine Kinase
6. In people with SD who have sicca (dryness) symptoms of the eyes, what is the most clinically effective topical treatment?
- Advise regular use of a preservative free lubricating eye drop (e.g. 2–3 hourly) (1, A) (SOA 94.4%).
- Autologous or allogeneic serum eye drops may be offered to individuals with ongoing symptoms despite maximal management with conventional eye drops (1, A) (SOA 91.9%).
- Topical steroid eye drops, under ophthalmic supervision, may be offered short term to individuals with ongoing persistent inflammation despite maximal management with conventional eye drops (1, A) (SOA 94.9%).
- Topical ciclosporin eye drops, under ophthalmic supervision, may be indicated for those with persistent surface inflammation despite maximal management with conventional eye drops (1, B) (SOA 94.9%).
- Punctal plugs are suitable in in certain circumstances, but they may make corneal surface inflammation worse in certain situations. Careful patient selection is important (1, C) SOA 96.3%.
7. In people with SD who have sicca (dryness) symptoms of the mouth, what is the most clinically effective topical treatment?
- Suggest saliva substitutes for symptomatic relief of oral dryness (2, C) (SOA 93.3%).
8. In people with SD who have sicca (dryness) symptoms outside the eyes and mouth, what is the most clinically effective topical treatment?
- Consider advising topical non-hormonal vaginal moisturizers plus oestrogen creams/pessaries in peri- or post-menopausal women with significant vaginal dryness (2, C) (SOA 97.5%).
9a. In people with SD who have sicca (dryness) symptoms, what is the most clinically effective stimulatory treatment?
- Consider a trial of pilocarpine (5 mg once daily increasing to 5 mg tds/qds) in those with significant ocular sicca symptoms with evidence of residual glandular function (1, A) (SOA 95.3%).
- Consider a trial of pilocarpine (5 mg once daily increasing to 5 mg tds/qds) in those with significant oral sicca symptoms with evidence of residual glandular function (1, A) (SOA 98.4%).
9b. What is the clinical effectiveness of fluoride, xylitol, chlorhexidine, artificial saliva or diet in preventing the development or progression of dental caries and gum disease?
- Recommend regular brushing with fluoride toothpaste, proactive dental care and the use of xylitol containing products as an alternative to sugar to prevent dental decay (2, C) (SOA 95.6%).
10a. In people with SD what is the clinical effectiveness of treatments in comparison to each other or placebo for treating systemic disease?
- In those with significant fatigue and systemic symptoms consider a trial of HCQ for 6–12 months (2, C) (SOA 95.6%).
- Systemic steroids may be used short term for specific indications but should not be offered routinely in the management of SD (2, C) (SOA 97.7%).
- Conventional immunosuppressive drugs are not routinely recommended for use in SD outside of the treatment of specific systemic complications (2, C) (SOA 94.7%).
- Biologic drugs are not currently recommended for use in SD outside of the treatment of specific systemic complications (2, C) (SOA 93.5%).
10b. What treatments are beneficial for recurrent parotitis in jSD?
- Treatment of parotitis in jSD (once infection and stone disease have been excluded) could include the following escalating therapies. A short course of NSAIDs or oral steroids combined with massage followed by washouts with saline or steroids. Consider anti-B-cell-targeted therapies in selected, refractory cases (2, C) (SOA 91%).
11. In people with SD, is early treatment of hypergammaglobulinaemia or systemic disease more effective than delayed treatment at slowing disease progression?
- In SD with significant hypergammaglobulinemia consider a trial of HCQ for 6–12 months (2, C) (SOA 94.2%).
12. What are the recommended therapeutic options in individuals with SD overlapping with other rheumatic diseases, for example, RA, SLE or scleroderma?
- In individuals with overlap CTDs take all confirmed disease entities into account when planning investigation and management (2, C) (SOA 96.3%).
13. In people with SD, what is the clinical effectiveness of nutraceuticals in the management of the condition?
- Consider vitamin A containing eye ointments (2, C) (SOA 89.8%).
- Consider advising omega-3 supplementation in SD (2, C) (SOA 89.8%).
(go to manuscript for full details and more recommendations)










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.