Long COVID Manifestations Save
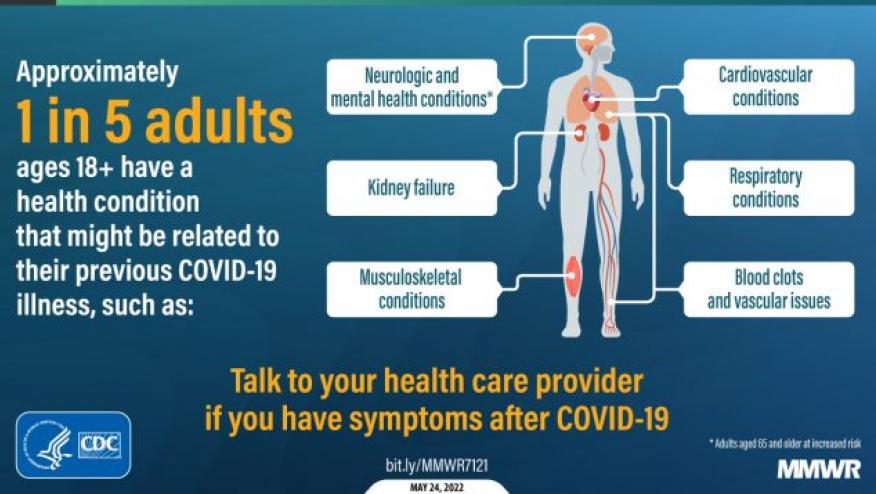
The acute consequences of a SARS-CoV-2 infection may be bothersome or devastating, but the long-term consequences may lead to so-called "long COVID" syndrome. Long COVID appears to affect up to 20% of those who survive COVID-19 infection.
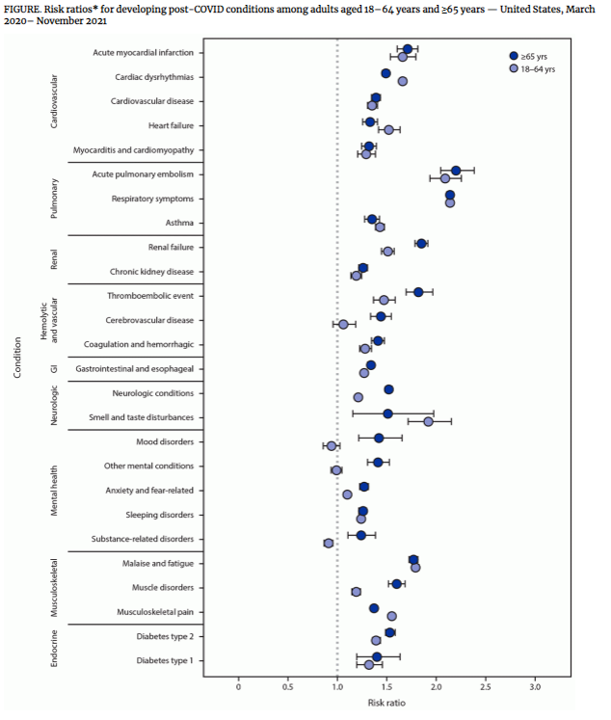
Persistent symptoms occurring ≥4 weeks after acute SARS-CoV-2 infection has been referred to as post-COVID conditions, or long COVID. CDC has used US electronic health record data (Cerner Real-World Data, a national, deidentified data set of approximately 63.4 million unique adult records; between March 2020–November 2021) to assess the incidence of 26 conditions (incident symptoms) often attributed to post-COVID and compared these symptoms to matched patients without evidence of COVID-19 in the EHR (control patients).
The recent MMWR reports that 38% of case-patients experienced at least incident condition (compared to 16% in controls) possibly affecting multiple systems (cardiovascular, pulmonary, hematologic, renal, endocrine, gastrointestinal, musculoskeletal, neurologic, and psychiatric).
The highest risk was seen for acute pulmonary embolism (RR = 2.1 and 2.2 among persons aged 18–64 and ≥65 years, respectively) and respiratory signs and symptoms (RR = 2.1 in both age groups).
Overall, one in five COVID-19 survivors aged 18–64 years and one in four survivors aged ≥65 years experienced at least one incident condition that might be attributable to previous COVID-19.
Among all patients aged ≥18 years, 38.2% of case-patients and 16.0% of controls experienced at least one incident condition - higher in the elderly ≥65 years, 45.4% of case-patients and 18.5% of controls experienced at least one incident condition. Depending on age, COVID-19 survivors had a 21% to 27% higher risk of long COVID symptoms.
In addition to common respiratory symptoms, cardiac and musculoskeletal symptoms were next most common. The RR for cardiac dysrhythmia was significantly higher among patients aged 18–64 years (RR = 1.7) compared with those aged ≥65 years (1.5). Similarly, the RR for musculoskeletal pain was higher among patients aged 18–64 years (1.6) then among those aged ≥65 years (1.4). Among case-patients, the RRs for 10 incident conditions was significantly higher among those aged ≥65 years than among those aged 18–64 years; these conditions were renal failure, thromboembolic events, cerebrovascular disease, type 2 diabetes, muscle disorders, neurologic conditions, and mental health conditions (including mood disorders, anxiety, other mental conditions, and substance-related disorders).
Awareness and research are needed to better understand and prevent long COVID manifestations.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.