Repetitive Transcranial Magnetic Stimulation in Fibromyalgia Save
A randomized, sham-controlled trial has shown that repetitive transcranial magnetic stimulation (rTMS) reduced pain in fibromyalgia for up to 8 weeks; while analgesic effects waned, functional improvements remained during extended maintenance at week 16.
This is the first randomised double-blind, sham-controlled trial to assess the efficacy of rTMS as an add-on therapy for fibromyalgia (FM). Study enrolled adult women with treatment refractory fibromyalgia and randomised them either to 10 Hz motor cortex (M1) rTMS, 3000 pulses day−1, or sham stimulation. This included 10 induction sessions over 2 weeks, followed by weekly maintenance (6 weeks), and fortnightly extended maintenance (8 weeks). Primary outcome was ≥50% pain reduction at week 8 compared with baseline. Secondary outcomes included pain interference, and Fibromyalgia Impact Questionnaire (FIQ) scores at weeks 8 and 16.
A totatl of 101 women (mean age 48 yr) to active (n=52) or sham (n=49) arms. The relative pain reduction was higher in the active than in the sham group (40.4% vs 18.4%, P=0.028) at week 8. At week 16, this probability reduced to 34.2% (OR 0.815; 95% CrI 0.313–2.1), but the likelihood of FIQ score reduction was 79.1%. The intervention appeared safe.
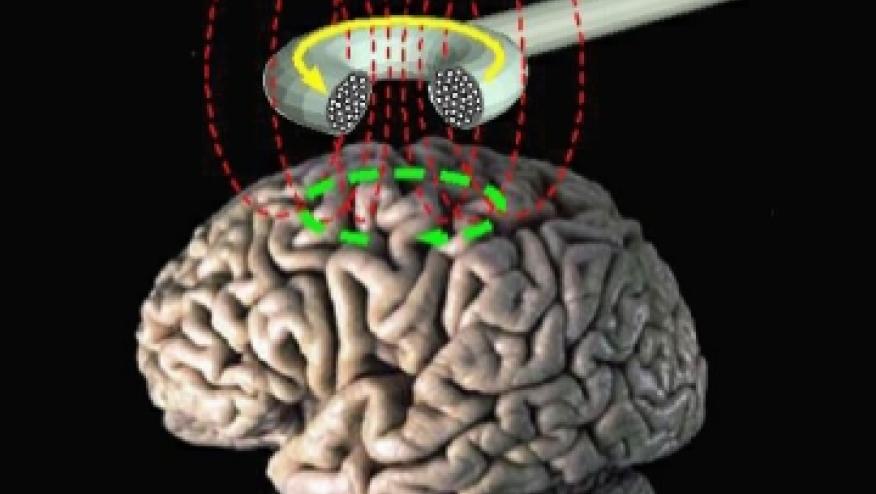
rTMS is a non-invasive brain stimulation technique that modulates cortical excitability and neural plasticity. Procedure involves an electromagnetic coil that is placed against the scalp, and magnetic pulses are delivered to stimulate the targeted brain area. The patient may feel a tapping sensation on the head. rTMS is generally considered a safe procedure, with minimal side effects.
Primary motor cortex stimulation with rTMS has been explored in other chronic pain conditions, mainly neuropathic pain, where it is currently indicated for use. Beyond voluntary motor control, M1 has areas that are highly connected to extra-motor networks responsible for interoceptive, cognitive, and nociceptive control. Analgesic effects are thought to depend on the release of endogenous opioids and the availability of NMDA-type glutamate receptors.
ADD THE FIRST COMMENT
Disclosures
The author has no conflicts of interest to disclose related to this subject










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.