Slow Lung Decline Typical in Systemic Sclerosis Save
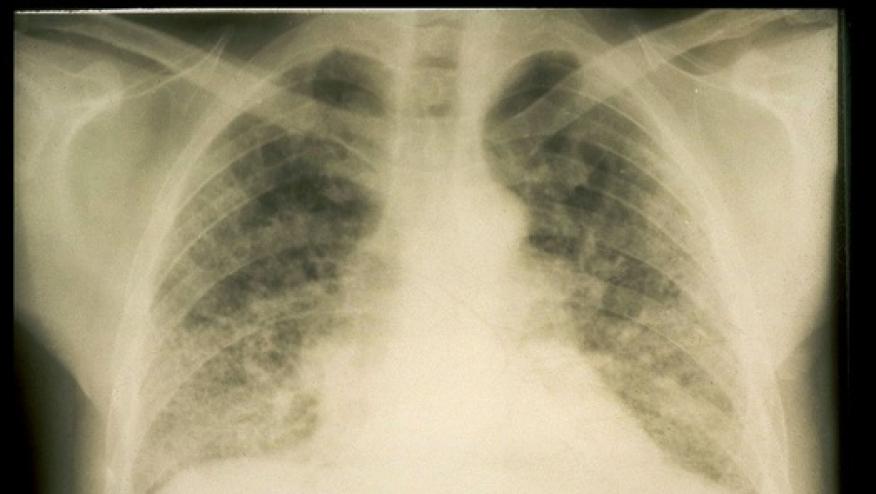
The interstitial lung disease that develops in a subset of patients with systemic sclerosis tends to be heterogeneous, with the majority of patients experiencing a slow pattern of decline in lung function, analysis of outcomes in the European Scleroderma Trials and Research (EUSTAR) database found.
Among patients with available lung function data for 12 months of follow-up, 12% had significant progression of decline in forced vital capacity (FVC), meaning a decline of more than 10%; 15% had moderate progression (decline of 5% to 10%); 48% were stable (decline or improvement of less than 5%); and 25% showed improvement (increase of 5% or more), noted Oliver Distler, MD, of University Hospital Zurich in Switzerland, and colleagues.
And over 5 years of follow-up, 58% of patients showed a slow pattern of decline, with more 12-month periods of stability or improvement than of decline, the researchers reported in their study online in Annals of the Rheumatic Diseases.
The proportion of patients with systemic sclerosis who develop interstitial lung disease and the pattern of disease progression have not been fully elucidated, and risk factors to predict who may be at high risk for progression and irreversible organ damage are uncertain. The availability of an approved treatment that can reduce the decline in lung function in systemic sclerosis (nintedanib, Ofev) highlights the unmet need of initiating treatment early, before lung fibrosis and damage has occurred.
To explore these concerns, Distler and colleagues assessed the prevalence, disease course, and risk factors among patients enrolled in EUSTAR since 2010.
Of the 6,004 patients with systemic sclerosis included in the database, 2,259 had imaging evidence of interstitial lung disease and 826 had lung function data for at least 12 months and were included in the analysis.
In a multivariate analysis, baseline factors that were associated with significant progression in lung disease at 12 months were:
- FVC, OR 1.02 (95% CI 1.01-1.03, P<0.001)
- Symptoms of reflux or dysphagia, OR 1.97 (95% CI 1.14-3.40, P=0.016)
- Modified Rodnan skin score, OR 1.06 (95% CI 1-1.12, P=0.036)
Among the 535 patients who had at least three FVC measurements over 5 years of follow-up, 9% had major declines of more than 20% in FVC; 14% had significant declines of 10-20%; 14% had moderate declines of 5-10%; 39% were stable, with changes of less than 5%; and 24% showed improvements.
During each 12-month period of the 5 years of follow-up, significant progression of interstitial lung disease was observed in 13-18%, and moderate progression in 9-10%. "These progressive periods rarely appeared in consecutive 12-month periods, and progressive periods were mostly followed by stable periods," the researchers noted.
Whereas 58% of patients showed a slow pattern of decline in FVC, a steadily progressive pattern, with more periods of decline than stability or improvement, was observed in 34% of patients, and in 8% a rapidly progressive course was seen, meaning consecutive periods of decline without intervening periods of stability or improvement.
In a multivariate linear mixed-effect regression analysis, baseline factors that were most strongly associated with progression over 5 years with significant interactions with time were:
- Male sex (R2 = -1.30, 95% CI -2.10 to -0.49, P=0.002)
- Symptoms of reflux or dysphagia (R2 = -0.72, 95% CI -1.34 to -0.10, P=0.024)
- High baseline Rodnan skin scores (R2 = -0.06, 95% CI -0.10 to -0.02, P=0.002)
Other baseline characteristics that were also associated with change in FVC decline but without a time interaction effect included older age, dyspnea, higher erythrocyte sedimentation rate, and higher diffusion capacity for carbon monoxide.
A total of 10% of patients died, with no significant differences in mortality rate according to progression of interstitial lung disease during the initial 12-month period or degree of decline over the 5 years of follow-up.
The observation that periods of decline could be preceded or followed by periods of stability or improvement could result in clinicians' underestimating the cumulative effects of lung function decline, according to the authors. "Smaller changes in FVC (5% to 10%) may in themselves be clinically significant, as seen in patients with idiopathic pulmonary fibrosis."
"In clinical practice, this means that FVC decline above 5% should alert physicians, especially when multiple declines occur, even when not in consecutive periods," the researchers stated, adding that it also emphasizes the importance of initiating treatment early to preserve lung function and of close monitoring of all patients with interstitial lung disease.
A limitation of the study, Distler and co-authors said, was the post-hoc design, although the data were collected prospectively.
The study was funded by Boehringer Ingelheim International.
Source Reference: Hoffmann-Vold A-M, et al "Progressive interstitial lung disease in patients with systemic sclerosis-associated interstitial lung disease in the EUSTAR database" Ann Rheum Dis 2020; doi:10.1136/annrheumdis-2020-217455.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.