Voclosporin FDA Approved for Lupus Nephritis Save

On January 22nd, the FDA approved voclosporin (Lupkynis) for use in adults with active lupus nephritis; voclosporin is a calcineurin-inhibitor immunosuppressant indicated for use in combination with a background immunosuppressive therapy.
FDA approval was based on data from the pivotal AURORA Phase 3 study and the AURA-LV Phase 2 study. These studies both demonstrated the ability of voclosporin to significantly improve LN outcomes after 52 weeks of followup in SLE nephritis patients receiving background standard of care (SOC) therapies like mycophenolate mofetil (MMF), and low dose steroids. In these pivotal trials, voclosporin treated patients were more than twice as likely to achieve renal response and experienced a decline in urine protein creatinine ratio (UPCR) twice as fast as patients on typical SoC alone.
Caveats from the Package Insert:
- Establish baseline renal function and blood pressure (not recommended if baseline eGFR ≤45 mL/min/1.73 m2 unless the benefit exceeds the risk; these patients may be at increased risk for acute and/or chronic nephrotoxicity).
- Recommended Doseage: starting dose: 23.7 mg orally q 12 hours (three 7.9 mg tablets bid)
- Use in combination with mycophenolate mofetil (MMF) and corticosteroids.
- Severe renal impairment: the recommended dose is 15.8 mg twice daily. Patients with mild and moderate hepatic impairment: the recommended dose is 15.8 mg twice daily
- Monitor BP and GFR
- Modify the dose based on eGFR - assess eGFR every two weeks for the first month, and every four weeks thereafter. If eGFR <60 mL/min/1.73 m2 and reduced from baseline by >20% and <30%, reduce the dose by 1 tab twice a day (meaning take 2 tabs bid) . Reassess eGFR within two weeks; if eGFR is still reduced from baseline by >20%, reduce the dose to just 1 tab (7.9 mg) twice a day.
- Monitor blood pressure every two weeks for the first month, and as clinically indicated thereafter. If BP >165/105 mmHg or with hypertensive emergency, discontinue voclosporin and initiate antihypertensive therapy.
- If NO CLINICAL BENEFIT by 24 weeks, consider discontinuation
- Drug interactions with strong CYP3A4 inhibitors (e.g., ketoconazole, itraconazole, clarithromycin).
- Warnings:
- Nephrotoxicity (with concomitant nephrotoxic drugs);
- Hypertension:
- Neurotoxicity: Including risk of posterior reversible encephalopathy syndrome (PRES)
- Hyperkalemia: monitor serum potassium levels
- QT Prolongation: Consider obtaining ECV in patients at high risk
- Avoid live vaccines.
- Pure Red Cell Aplasia
- Common adverse effects: GFR decreased, hypertension, diarrhea, headache, anemia, cough, urinary tract infection, abdominal pain upper, dyspepsia, alopecia, renal impairment, abdominal pain, mouth ulceration, fatigue, tremor, acute kidney injury, and decreased appetit
- Not recommended in patients with a baseline eGFR ≤45 mL/min/1.73 m2, unless the benefit exceeds the risk.
- With severe renal impairment at baseline, voclosporin should be used at a reduced dose.
- Mild and moderate hepatic impairment: Dose reduction is required. If there is severe hepatic impairment: Avoid voclosporin use
In both studies, a total of 533 patients with LN were randomized to receive either LUPKYNIS 23.7 mg or placebo twice daily used with SoC. All patients were dosed with concurrent MMF at a target dose 2 g/day. In both studies, initial treatment with intravenous (IV) methylprednisolone up to a cumulative dose of 1 g was administered on Days 1 and 2, and all patients received a subsequent taper of oral corticosteroids. The starting dose of oral prednisone was 20 mg/day for patients with a body weight of <45 kg and 25 mg/day for patients ≥45 kg. The dose of oral corticosteroid was tapered down to achieve a target dose of 2.5 mg/day by Week 16. The studies enrolled patients with LN of Class III or IV (alone or in combination with Class V) or pure Class V. Enrolled patients were required to have baseline eGFR >45 mL/min/1.73 m2.
In the Phase 3 study, at one year, LUPKYNIS plus SoC was more than two times as effective at achieving a complete renal response than the SoC alone. Patients in the study taking LUPKYNIS also achieved a 50 percent reduction in UPCR twice as fast as SoC, and a higher portion of LUPKYNIS-treated patients achieved a complete renal response at 24 weeks compared to patients receiving SoC. The study results were achieved using a protocol-defined steroid taper. Patients treated with LUPKYNIS showed improved response rates in all parameters across immunologically-active classes of LN studied.
The most common adverse reactions (>3%) were glomerular filtration rate decreased, hypertension, diarrhea, headache, anemia, cough, urinary tract infection, abdominal pain upper, dyspepsia, alopecia, renal impairment, abdominal pain, mouth ulceration, fatigue, tremor, acute kidney injury, and decreased appetite.
Voclosporin was approved by the FDA under Priority Review and was previously granted Fast Track designation from the Agency in 2016.
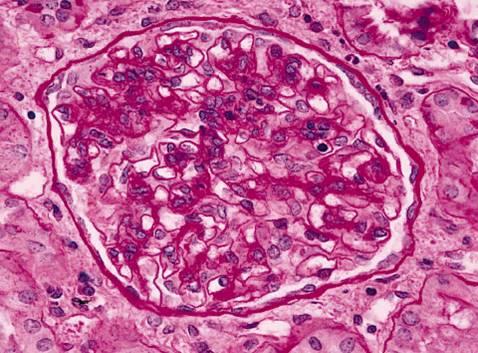
Systemic lupus erythematosus (SLE) affects 200,000-300,000 people in the U.S. and approximately one-third will develop LN. Black and Hispanic individuals with SLE also tend to develop LN earlier and have poorer outcomes when compared to Caucasian individuals.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.