Why Depression Screening Should be Mandatory at Each Visit Save

- Comorbid Depression impairs potential drug responses (regardless of diagnosis)
- Patients with Comorbid Depression have more pain, more ER visits, more healthcare costs
- A patients with comorbid depression have a higher death rate
- Depression goes unrecognized in outpatient rheumatology clinics.
Depression is more widespread than ever in the United States, according to a new study from Gallup, showing that 18% of adults are depressed (or receiving depression treatment for depression) – an increase in 7 percentage points since 2015. In the USA, the lifetime risk of depression is 29%, also increased (10%) since 2015.
In the U.S., provider-diagnosed arthritis (arthritis) affects 54.4 million (22.7%) and is supposed to rise to 78.4 million by 2040. Chronic painful conditions like arthritis commonly are complicated by poor mental health, anxiety and depression; all of which can worsen patient quality of life and outcomes.
The CDC estimated that 19% of U.S. adults have a history of depression (based on the 2017 Behavioral Risk Factor Surveillance System; BRFSS). The median age-adjusted prevalence of depression among adults with arthritis was 32.1% (ranging from 17.7% in Hawaii to 36.6% in Oklahoma).
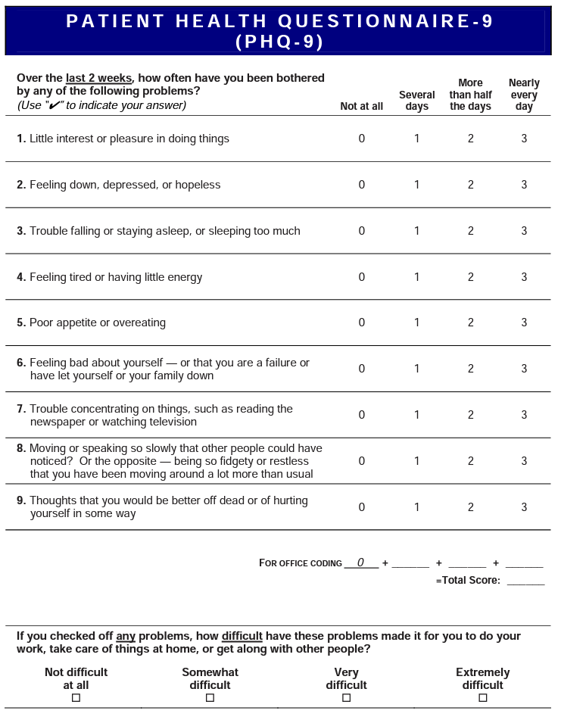
A 2022 Cochrane analysis 173 studies, 8.5 million persons) showed that depression screening interventions were associated with a lower prevalence of depression after 6-12 months (OR, 0.60 [95% CI, 0.50 to 0.73]. Screening interventions included patient health questionnaire (PHQ-2 followed by the full PHQ-9 if the PHQ-2 is positive). As expected, abnormal screening results followed by psychological and pharmacologic treatment of depression were beneficial.
The consequences of chronic pain and disability are well known to rheumatologists and include poor sleep, and fibromyalgia that may escalate or contribute to depression. Moreover, the presence of anxiety and depression are associated with poorer overall health and quality of life.
Following the pandemic (from August 2020 to February 2021) the frequency of anxiety or depressive symptoms increased from 36% to 41.5%. According to the World Health Organization, anxiety and depression increased by 25 percent globally during the first year of the pandemic.
Depression Facts
- Number of physician office visits with depressive disorders as the primary diagnosis: 15.0 million
- Percent of physician office visits with depression indicated on the medical record: 11.0%
- Depression was found in 30% of psoriatic arthritis patients (n=208); higher in those with higher disease activity (DAPSA; P=.007) and functional impairment (HAQ-DI; p=-.02)
- In one study of 182 adult RA patients, half had depression and 25% had anxiety. Patients with depression or anxiety had higher HAQ and DAS28 scores. Depression was more prevalent in females, housewives, and those with low education. Anxiety was more prevalent in blue-collar workers
- A recent report from the DANBIO registry of RA patients has shown that depression is associated with a 3-fold higher risk of all-cause mortality.
- RA patients have an increased (50-60%) risk of post-partum depression in women without a prior psychiatric history.
- There is a bidirectional association between depression and RA (or SLE) – meaning those with depression have a higher risk of RA and SLE; and patients with RA or SLE have a higher risk of depression.
- A study of 2976 OA patients followed for 3 years, showed half had moderate‐to‐severe pain, 54% had subclinical or clinical insomnia, and 45% had subclinical or current depression.
- Study of 148 JIA patients (median age 14.7 years) found the prevalence of depressive symptoms was 13% and for depression 9.5%, of which 71.4% were newly identified with depression https://pubmed.ncbi.nlm.nih.gov/37039854/
The U.S. Preventive Services Task Force has recommended that medical practitioners actively screen and identify anxiety and depression in all adult patients under 65 yrs.
Screening is simple, time efficient and can lead to substantial patient benefits if depression (or anxiety) is identified early and managed effectively.
3 Ways to screen for depression.
- Ask the patient, “have you experienced depression in the last 2 weeks?”
- Use the RheumNow Followup Clinic Visit Survey (includes 2 check boxes for depression)
- Include the PHQ-9 Screener form for patients to fill out. (Scores of 5, 10, 15, and 20 represent cutpoints for mild, moderate, moderately severe and severe depression, respectively). There is a shorter PHQ-2 screener.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.