Biologics Beneficial in Eosinophilic Vasculitis Save
Two biologic therapies showed promise in the treatment of refractory or relapsing eosinophilic granulomatosis with polyangiitis (EGPA) in a retrospective European study.
Among 63 patients who were treated with rituximab (Rituxan), remission or partial responses at 1 year were observed in 49% and 24% of patients, respectively, reported Benjamin Terrier, MD, PhD, of Université Paris Descartes in Paris, and colleagues.
In addition, as shown in the team's study online in Arthritis & Rheumatology, among the 51 patients who had received mepolizumab (Nucala), remission or partial response at 1 year was seen in 78% and 10%, respectively. Remission or partial response was seen in only 15% and 33% of the 33 patients treated with omalizumab (Xolair).
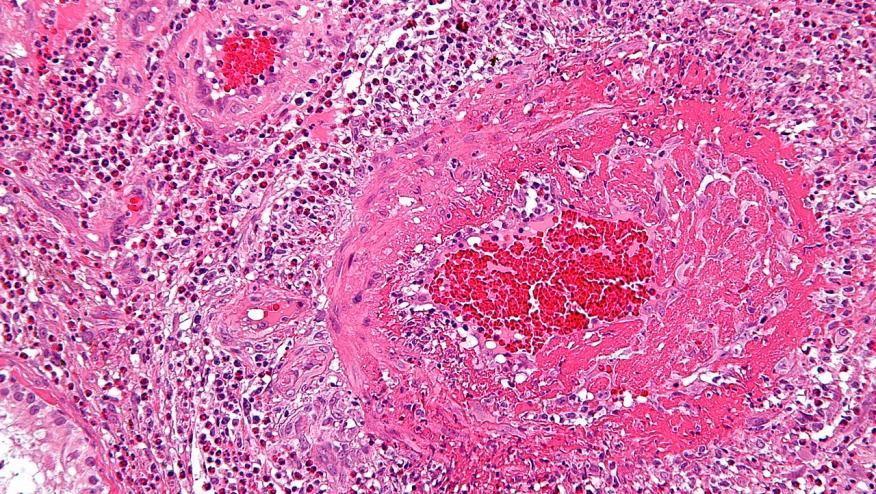
EGPA is a small-vessel vasculitis characterized by asthma, sinusitis, and blood and tissue eosinophilia, with a subset of patients also positive for antineutrophil cytoplasmic antibodies (ANCA). Traditional therapy has relied on glucocorticoids and conventional immunosuppressants, but relapses are common and long-term use of steroids carries significant risk.
"Because EGPA shares pathophysiological features with other ANCA-associated vasculitides, eosinophilic disorders, and asthma, alternative therapeutic options may be considered in EGPA, especially rituximab (monoclonal anti-CD20 antibody), omalizumab (monoclonal anti-IgE antibody) and mepolizumab (monoclonal anti-IL[interleukin]-5 antibody)," the researchers wrote.
Rituximab is indicated for use in rheumatoid arthritis, granulomatosis with polyangiitis, and microscopic polyangiitis, and omalizumab is indicated for asthma and chronic idiopathic urticaria.
Mepolizumab was approved for the treatment of EGPA in the U.S. in December 2017 after efficacy was demonstrated in a phase III trial, but has not been approved for this indication in Europe.
To examine the European experience with these agents, Terrier and co-authors conducted a collaborative study of patients who had received biologic therapy for vasculitis flares, refractory eosinophilic asthma, and ear, nose, and throat manifestations.
Remission was defined as a Birmingham Vasculitis Activity Score (BVAS) of zero and a daily prednisone dose of 5 mg or less, and partial response was a score of zero and prednisone dose of 6-10 mg/day. Outcomes other than remission and partial response included treatment failure and stopping treatment due to adverse events.
Rituximab was given in doses of 1,000 mg 2 weeks apart or 375 mg/m2/week for four infusions; mepolizumab was given in monthly doses of 100 or 300 mg. Omalizumab typically is given every 2 or 4 weeks, with dosing determined according to patient age, weight, and IgE level, the researchers noted.
Rituximab was most commonly given for vasculitis flares, although these were often accompanied by asthma, while mepolizumab and omalizumab were initiated for glucocorticoid-dependent asthma and ear, nose, and throat manifestations.
Among the rituximab-treated group, the median BVAS declined from 8.5 at baseline to 1 at 6 months and 0 at 12 months, and median prednisone dosages declined from 20 mg/day to 7.5 mg/day at 6 and 12 months, respectively. Therapeutic failure was observed in 24% of patients and withdrawal due to adverse events in 3%.
Remission was reported in 59% of patients who were ANCA positive and 41% of those who were ANCA negative.
"Overall, rituximab seems to be an acceptable alternative agent in vasculitis manifestations, but the benefit/risk ratio remains to be evaluated in randomized controlled trials," two of which are ongoing, the researchers noted.
The glucocorticoid-sparing effects of mepolizumab was notably superior with mepolizumab compared with omalizumab, the investigators pointed out. With mepolizumab, median dosages fell from 10 mg/day at baseline to 5 mg/day at 6 months and 3.9 mg/day at 12 months, compared with a decrease from 15 mg/day to 11 mg/day at 6 months and 10 mg/day at 12 months with omalizumab.
Median BVAS decreased from 2 at baseline in the mepolizumab group to 0 at both 6 and 12 months, and from 2 to 1 at 6 months and then 0 at 12 months in the omalizumab group.
Treatment failures and adverse event withdrawals were observed in 8% and 4%, respectively, with mepolizumab and in 48% and 4% with omalizumab, the researchers reported.
Remission rates were 82% at 12 months among patients given mepolizumab with the 300 mg dose (standard dose) and 76% with the lower 100 mg dose -- "suggesting that 100 mg could be an acceptable dose at first line, with the possibility to increase to 300 mg monthly in case of inadequate response," Terrier and co-authors stated.
A total of 16 patients discontinued rituximab, two because of severe adverse events and 14 because of treatment failure. In addition, 17 patients reported adverse events, which most commonly were moderate to severe infections.
Omalizumab was discontinued in 17 patients, due to treatment failure in 16 and adverse events in one. Four patients reported mild or moderate adverse events.
Three patients stopped mepolizumab because of severe adverse events in two and pregnancy in one. Eleven patients reported mild or moderate adverse events, most commonly asthenia.
"Overall, these data clearly reinforce the key message that omalizumab has low efficacy in EGPA, unlike mepolizumab and potentially other IL-5-targeting therapies," the researchers concluded, adding that the 100 mg dose of mepolizumab has yet to be directly compared with the validated 300 mg monthly dose.
Source Reference: Canzian A, et al "Use of biologics to treat relapsing and/or refractory eosinophilic granulomatosis with polyangiitis: data from a European collaborative study" Arthritis Rheum 2020; doi:10.1002/art.41534.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.