EULAR 2023 – Day 1 Report Save
EULAR 2023 launched today to crowds of attendees. The opening Plenary session and presidential address by Dr. Ian McInnes was followed by a number of overview and review sessions with but a half-day of abstracts presentations, on several therapeutic areas including osteoarthritis, JIA, COVID and more. The following are a few of the presentations that caught my eye.
- Certainty of an Axial Spondyloarthritis (axSpA) diagnosis. Abstract OP0005 examined data from the SPACE cohort study that enrolled 555 patients with new onset chronic low back pain (>3 mos., but <2 years). These patients were assessed by the rheumatologist at baseline, 3 months, 1 and 2 years. At baseline 32% were diagnosed with axSpA. The good news is that very few patients had a change in diagnosis, such that at 2 years 30% were still axSpA. The authors stressed that a firm diagnosis was had at baseline (or by 3 months) based on rheumatology referral, history, exam with HLA-B27 and imaging being most discriminatory. These data confirm the accuracy of the rheumatologist in diagnosing axSpA and that only 15% of patients presenting with chronic low back pain remain uncertain over time.
- Denosumab in Erosive Hand OA. Abstract OP0071 was originally presented at ACR 2022 with the takeaway message that denosumab (DEN) prevents erosive change in hand OA progression and new erosions, but doesn't affect pain at 48 weeks. This extended report adds on two-year outcome data. Essentially, 100 HOA patients were given either placebo or DEN Q3 months. The primary endpoint was erosive hand OA X-ray outcomes (GUSS scores) at week 24 and 48. Thereafter, placebo pts rolled over to DEN for another year. The new revelation here was that a pain benefit was finally seen at week 96 in the DEN treated patients. Thus, begging the question, is this real? Why so delayed? Is this compelling enough to use DEN, primarily for structure modification in erosive hand OA and would you do so early in the disease to get the x-ray benefit with an unclear promise of pain relief from the RANK ligand inhibitor alone. These findings are exciting, but clinical application is questionable.
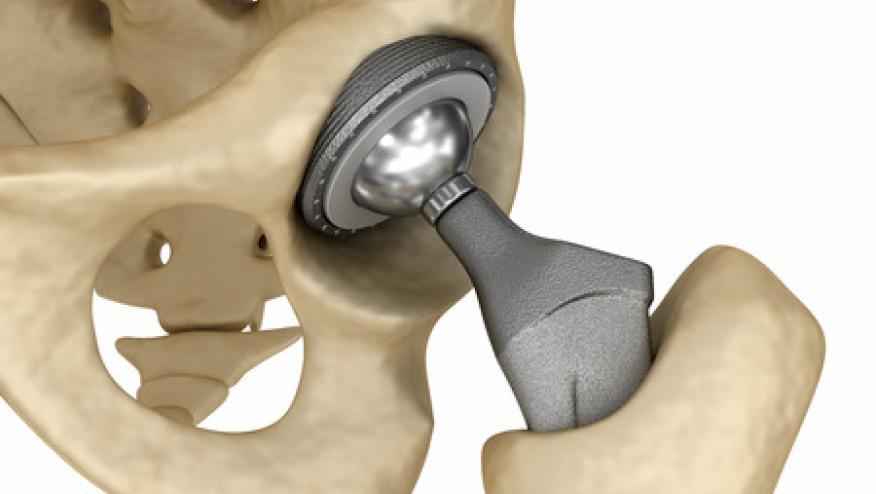
- Low Dose Colchicine – Can it Reduce the Risk of TKR & THR? Abstract OP0072 by Heijman, et al. presented the results of the low dose colchicine 2 (LoDoCo2) previously published in the NEJM in 2020. LoDoCo2 randomized >5400 patients with chronic coronary artery disease to receive either placebo or colchicine 0.5 mg qd. The study demonstrated a significant reduction in subsequent CV events in those treated with colchicine. This research presented today, was also just published in the Annals of Internal Medicine. This was a retrospective, exploratory subanalysis of a data set no originally intended to study OA outcomes or the need for hip or knee replacement surgery. Despite not having any baseline data on OA prevalence, joint pain, arthritis meds, this study showed that colchicine use was associated with a 31-40% lower risk of future TKR/THR. While these results are impressive, the putative protective effects of colchicine are at odds with all the other data showing that colchicine has little or no effect in osteoarthritis of the hand and knee outcomes. Nonetheless this study should get some buzz from the meeting and the press.
ADD THE FIRST COMMENT
Disclosures
The author has no conflicts of interest to disclose related to this subject










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.