EULAR/ACR Classification in MDA5+ Myositis Patients Save
The diagnosis of idiopathic inflammatory myopathies (IIMs) can be informed by the 2017 EULAR/ACR classification criteria, but their utility in patients with clinically amyopathic dermatomyositis (CADM) and anti–melanoma differentiation–associated protein 5 (anti–MDA-5)–positive IIM is less certain. A current analysis suggests that nearly 30% of MDA5 IIM patients may be missed by the 2017 EULAR/ACR classification criteria for IIM.
A total of 120 consecutive adult patients diagnosed as having anti–MDA-5–positive IIM from 10 Hong Kong hospitals were studied. One-third (31.7%) had dermatomyositis, and two-thirds (68.3%) had CADM. An IIM diagnosis was found in 72% using EULAR/ACR criteria and 41% using Bohan and Peter criteria.
The sensitivity of the EULAR/ACR criteria could be improved to 98.3% if anti–MDA-5 antibody–positive status was considered as one of the criteria. The MSA-based criteria had 100% sensitivity. With modification of specific phenotypic-serologic criteria to capture classification of patients with anti–MDA-5 antibodies, 97.5% of patients were able to be classified as having IIM.
Studies have shown the EULAR/ACR criteria had a higher sensitivity (87.7%) compared to the Bohan and Peter (BP) criteria (80.4%) and that the EULAR/ACR criteria specificity was very high (>98%) for the major IIM subgroups polymyositis, dermatomyositis, and inclusion body myositis.
In a previous report it was shown that in myositis patients with MSAs, autoantibodies outperform the EULAR/ACR-defined myositis subgroups in predicting the clinical phenotypes of patients - suggesting that MSAs should be included in future revisions of the myositis classification scheme.
These authors suggest incorporating anti–MDA-5 antibody positivity as a criterion into existing or future criteria sets to diagnose patients with IIM.
The EULAR/ACR Classification Criteria for Adult and Juvenile Idiopathic Inflammatory Myopathies and their Major Subgroups
(suggested total aggregated score of score of ≥5.5 and ≤ 5.7 (≥6.7 and ≤ 7.6 if biopsy is available)
| Variable | Score Points | |
|---|---|---|
| Without muscle biopsy | With muscle biopsy | |
| Age of onset | ||
| Age of onset of first symptom assumed to be related to the disease ≥ 18 years and < 40 years | 1.3 | 1.5 |
| Age of onset of first symptom assumed to be related to the disease ≥ 40 years | 2.1 | 2.2 |
| Muscle weakness | ||
| Objective symmetric weakness, usually progressive, of the proximal upper extremities | 0.7 | 0.7 |
| Objective symmetric weakness, usually progressive, of the proximal lower extremities | 0.8 | 0.5 |
| Neck flexors are relatively weaker than neck extensors | 1.9 | 1.6 |
| In the legs proximal muscles are relatively weaker than distal muscles | 0.9 | 1.2 |
| Skin manifestations | ||
| Heliotrope rash | 3.1 | 3.2 |
| Gottron´s papules | 2.1 | 2.7 |
| Gottron’s sign | 3.3 | 3.7 |
| Other clinical manifestations | ||
| Dysphagia or esophageal dysmotility | 0.7 | 0.6 |
| Laboratory measurements | ||
| Anti-Jo-1 (anti-histidyl-tRNA synthetase) autoantibody present | 3.9 | 3.8 |
| Elevated serum levels of creatine kinase (CK)* or lactate dehydrogenase (LDH)* or aspartate aminotransferase (ASAT/AST/SGOT)* or alanine aminotransferase (ALAT/ALT/SGPT)* | 1.3 | 1.4 |
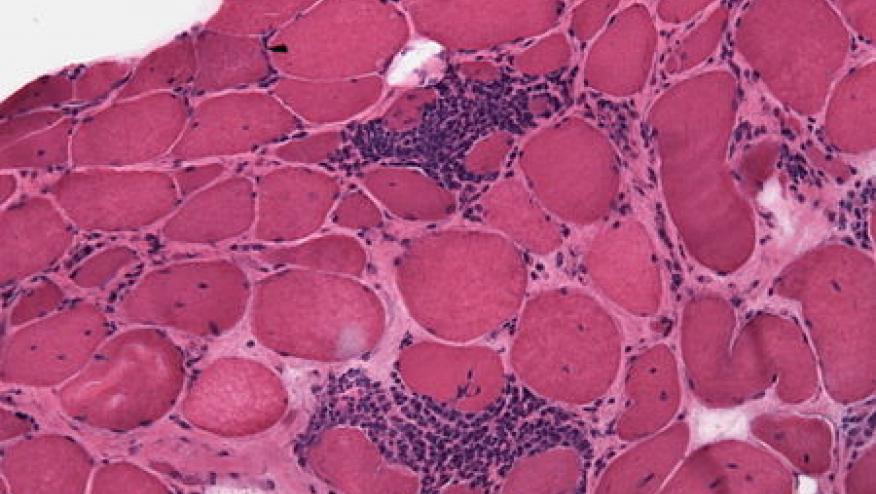
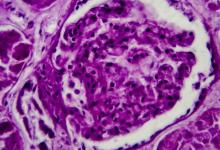
| Muscle biopsy features- presence of: | ||
| Endomysial infiltration of mononuclear cells surrounding, but not invading, myofibres | 1.7 | |
| Perimysial and/or perivascular infiltration of mononuclear cells | 1.2 | |
| Perifascicular atrophy | 1.9 | |
| Rimmed vacuoles | 3.1 | |








If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.