Rheumatologists and the Early Diagnosis of Spondyloarthritis Save
SPACE study of adults referred to rheumatology with less than 2 years of chronic back pain (CBP), shows that only one-third can be reliably diagnosed with axial spondyloarthritis (axSpA).
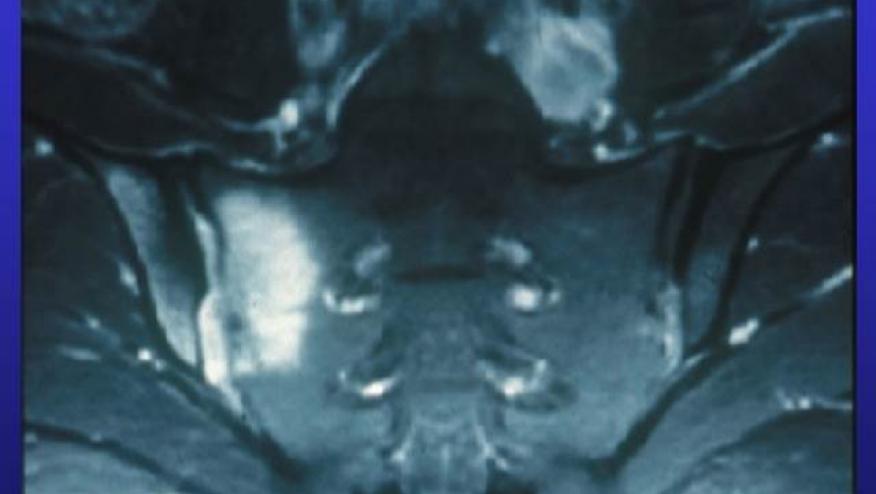
Data from SPondyloArthritis Caught Early European cohort of early CBP patients (<45 years; Sxs ≥3 months, ≤2y) of unknown origin. Such patients were repeatedly evaluated clinically, radiographically (radiographs and MRI) along with serologies and HLA-B27. The main outcome was the diagnosis of axSpA diagnosis at 2yrs.
The total included 552 patients with CBP, from which 175 (32%) were diagnosed with axSpA at baseline and another 165 (30%) at 2yrs. From baseline, the axSpA diagnosis was revised in 5% of patients. Overall, diagnostic uncertainty persisted in 30%.
Best predictors of a 2 year diagnosis axSpA was HLA-B27+ and baseline sacroiliitis imaging.
Over 2 years 8 patients developed MRI-sacroiliitis; 7/8 were HLA-B27+ and 5/8 male.
The diagnosis of axSpA can be reliably made in nearly one-third of patients with CBP upon presentation to the rheumatologist; and with time another 5%–30% may evolve into axSpA by 2y. The value of repeat MRI of the SI is modest but may be worthwhile in male HLA-B27+ patients.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.