Infectious Sacroiliitis Save
A large Chinese cohort study of patients with infectious sacroiliitis (SI) suggests that CT-guided biopsy of the sacroiliac joint is necessary to properly identify the infectious pathogen leading to SI.
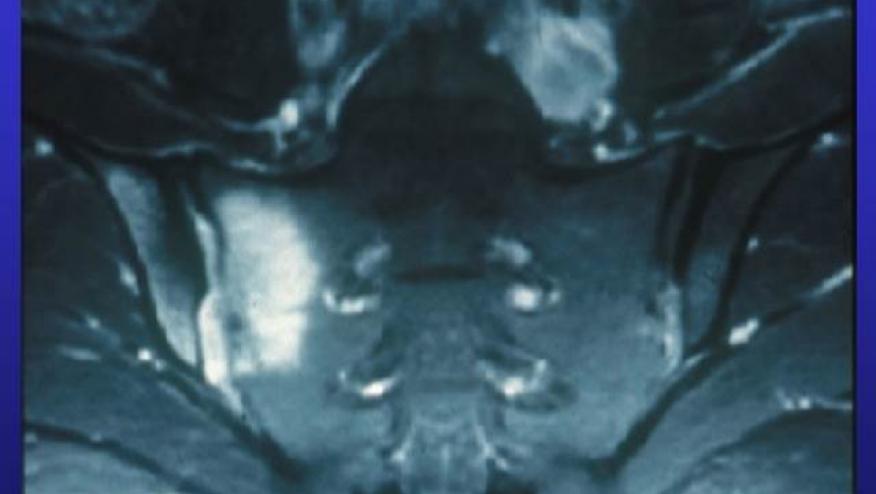
This retrospective analysis included 135 patients diagnosed between 2008 and 2020. Diagnoses were based on clinical features, labs, pathological and magnetic resonance images (MRI) results.
The diagnoses included:
- Pyogenic sacroiliitis (PSI) - 67%
- Tuberculous sacroiliitis (TSI) - 21%
- Brucellas sacroiliitis (BSI) - 13%
Nearly half (51%) of these patients met ASAS criteria for axial spondyloarthritis.
Interestingly, reports of back pain was lower in PSI (19%) than TSI (39%) and BSI (65%) groups.
Common MRI findings included sacroiliac joint erosion and bone marrow edema. Higher erythrocyte sedimentation rate (ESR) was seen in PSI (53 ± 29.63 mm/h) and TSI (56 ± 19.39 mm/h) compared to BSI patients (33 ± 25.12 mm/h).
All patients underwent CT-guided sacroiliac joint biopsy, with 87% having had positive results through tissue culture and pathological examination. Only 2 patients were diagnosed through blood culture, and one other diagnosed through the brucellosis agglutination test.
Infectious SI may mimic spondyloarthritis, and may have atypical features on imaging and clinical parameters. Infectious sacroiliitis should be suspected, especially in female patients, in patients who are HLA-B27 negative and who manifest fever, elevated ESR, or unilateral lesions on imaging.
• This study provides insights into the clinical and imaging features of infectious sacroiliitis based on a large number of cases.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.