Venous Thromboembolic Risk with Joint Replacement Save
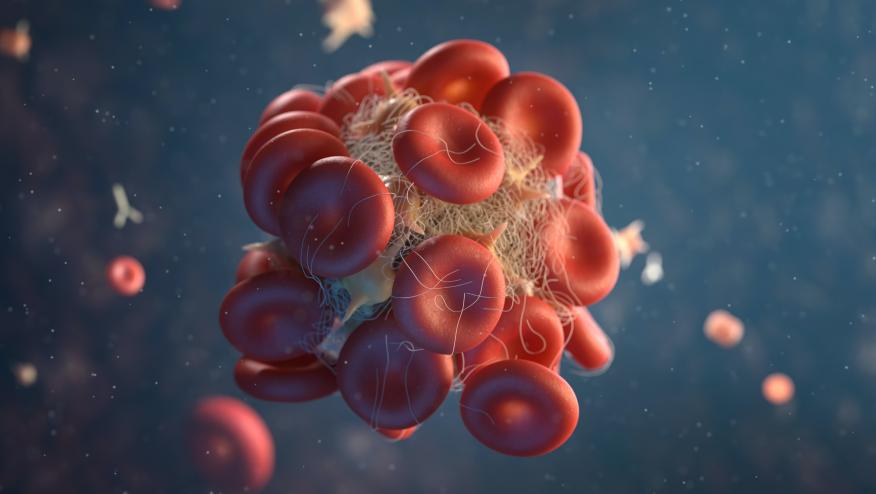
The role of thromboprophylaxis following total hip (THA) or total knee arthroplasty (TKA) is uncertain and consensus is lacking. A recent study suggests that thromboprophylaxis strategies should be tailored to individual risk of thrombosis and bleeding.
This retrospective cohort study used data from a large health care claims database to assess the risk of postoperative venous thromboembolism (VTE) and bleeding in THA or TKR patients using different thromboprophylaxis measures (aspirin, apixaban, rivaroxaban, enoxaparin, or warfarin). In this propensity-matched analysis, patients receiving a direct oral anticoagulant (DOAC) were matched with those receiving aspirin. Patients on anticoagulants before surgery were excluded. The primary outcome was 30-day cumulative incidence of post discharge VTE and post discharge bleeding (secondary).
Among a total of 29 264 patients, the median age was 59 (55-63) years, 58% were female, 37% had THA and 63% underwent TKA. The cumulative 30 day VTE incidence was 1.19% and the cumulative incidence of bleeding was 3.43%.
The leading risk factors for VTE risk included:
- prior VTE history (odds ratio 5.94 [95% CI, 4.29-8.24]),
- hereditary hypercoagulable state (OR, 2.64 [95% CI, 1.32-5.28]),
- knee arthroplasty (OR, 1.65 [95% CI, 1.29-2.10]),
- male sex (OR, 1.34 [95% CI, 1.08-1.67]).
In the propensity-matched cohort of 7844 DOAC-aspirin pairs, there was no significant difference in the risk of VTE in the first 30 days after the surgical procedure (OR, 1.14 [95% CI, 0.82-1.59]), but postoperative bleeding was more frequent in patients receiving DOACs (OR, 1.36 [95% CI, 1.13-1.62]).
Patients undergoing total hip or total knee arthroplasty, patient risk factors, (not choice of aspirin or DOAC), drive the risk of postsurgical VTE.
Postoperative bleeding rates were lower in patients prescribed aspirin.
Thromboprophylaxis strategies should be patient-centric and tailored to each patients individual risk.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.