A Review of Relapsing Polychondritis Save
A current review in the Journal of Thoracic Disease on relapsing polychondritis (RP), suggests that while this rare disorder may have an uncertain pathogenesis, its diagnosis and therapeutical management has improved.
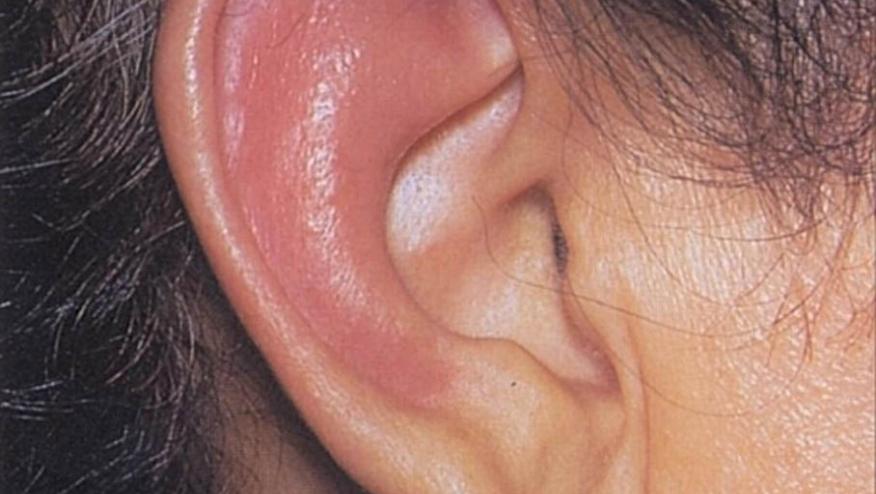
This review focuses on key features, with damage to auricular or nasal cartilage, and tracheobronchial and cardiac involvement that can be severe, and life threatening.
Tracheobronchial involvement can be assessed by dynamic thoracic imaging, flexible bronchoscopy and assessment of pulmonary function (with new emphasis on pulse oscillometry). Nuclear imaging can help with detection of metabolic activity on involved cartilages, leading to sharpen the final diagnosis.
- RP mainly affects adults, with a peak age at diagnosis between 40 to 50 years old (range 2 to 84 years)
- Tracheobronchial chondritis occurs in 60% of RP patients, characterized by cough and progressive dyspnea. Inflammation and cartilaginous destruction may lead to malacia, stenosis, and/or bronchiectasis, and infectious complications
- VEXAS patients are often mislabeled as RP
- Differential Dx for RP includes: VEXAS, GPA, IBD, Sarcoidosis, Pemphigoid, IgG4 related disease, Tracheobronchial amyloidosis, etc.
- Treatment approaches include respiratory support, surgical interventions, high dose steroids, and immunosuppressives (cyclophosphamide, methotrexate, azathioprine mycophenolate mofetil) are often used. There is limited data on the use of TNF inhibitors, tocilizumab and abatacept.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.