2025 ACR Guideline for the Treatment of SLE Save
The ACR has released its 2025 Systemic Lupus Erythematosus (SLE) treatment guidelines and consensus-based good practice statements, applicable to children and adults with SLE.
Overall, the goals of SLE management are to achieve remission or a low level disease activity, reduce morbidity and mortality, and minimize treatment-related adverse events.
For treatment of SLE, they recommend universal use of hydroxychloroquine, minimizing glucocorticoid exposure, and early introduction of conventional and/or biologic immunosuppressive therapies.
They strongly emphasize the role of shared decision-making between patients and clinicians, and collaborative care between rheumatologists and other specialists.
Recommendations were rated by consensus as being either Strong or Conditional (expert opinion). Unfortunately the level of evidence for nearly all of their recommendations is either very low or low.
Good Clinical Practice Statements
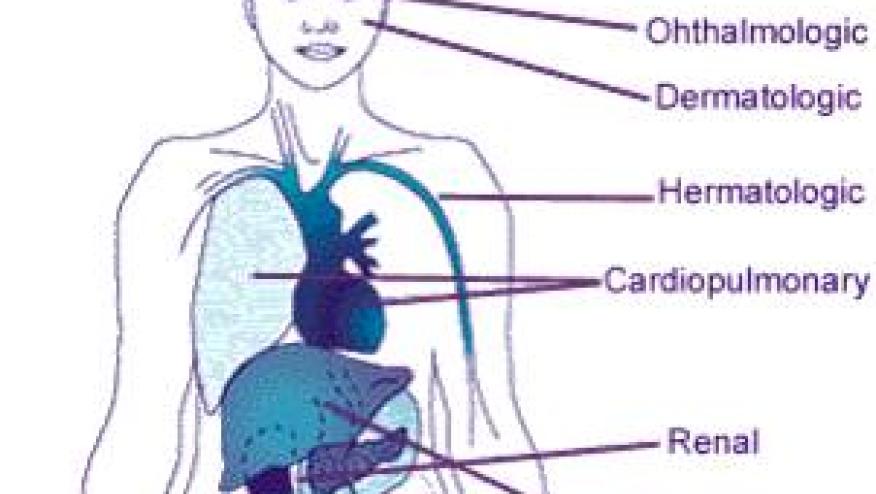
- All people with SLE should receive screening, monitoring, and management for comorbid conditions associated with SLE and its therapies (including infection, cardiovascular disease, bone and joint damage, malignancy, reproductive health complications, and presence of antiphospholipid antibodies.
- The goal of SLE treatment should be optimal control of disease (e.g., remission or a low level of disease activity) to improve long-term clinical outcomes.
- Prescribe glucocorticoids promptly to obtain rapid control of acute inflammation using the lowest dose and shortest duration necessary and initiate immunosuppressive therapy early to minimize glucocorticoid-related toxicity.
- People with active SLE symptoms should be diagnosed and treated promptly, with severity of lupus activity guiding intensity and choice of therapy.
- When multiple organ systems are involved at onset or during a flare of SLE, therapy should be directed toward all manifestations but should prioritize areas at greatest risk for irreversible damage.
- Organ- or life-threatening SLE should be treated urgently/emergently with aggressive therapy (e.g., pulse/high-dose glucocorticoid and immunosuppressive therapy), including consideration of combination therapies, as time may not permit sequential therapy; the clinical situation and patient’s preference should guide the specific combination therapy.
- When medications, procedures, and surgeries beyond the scope of rheumatology practice are considered, the decision to proceed with such therapies requires multidisciplinary discussion between the rheumatologist and the relevant specialists/proceduralists/surgeons.
- When clinical or serologic findings suggest an additional diagnosis or overlap with SLE (e.g., aquaporin-4 antibodies in setting of known SLE and new onset transverse myelitis or optic neuritis), therapy should be adjusted if necessary, depending upon which process is predominant and in consultation with the relevant specialist(s).
- People with SLE should be educated on the use of sunscreen and other sun-protection measures to reduce risk of rash and potential disease flare.
- Initial therapy for cutaneous lupus rash—in addition to HCQ—should be topical, including glucocorticoid and/or calcineurin inhibitors; initial therapy may also include a course of intralesional glucocorticoid with dermatology and/or a brief, limited course of oral glucocorticoid.
- Initial therapy for acute or recurrent episodes of inflammatory arthritis in people with SLE may include a course of NSAID or a limited course of oral glucocorticoid while waiting for recommended long-term therapies to take effect.
Strong Recommendations (there were but a few)
- In people with SLE with stable controlled SLE on prednisone >5 mg/day: ...We strongly recommend tapering the prednisone to a dose of ≤5 mg daily (and ideally to zero) within 6 months.
- In people with SLE with stable controlled SLE on prednisone >5 mg/day: ...We strongly recommend tapering the prednisone to a dose of ≤5 mg daily (and ideally to zero) within 6 months.
- For ongoing SLE disease activity in any organ system(s) refractory to initial therapy, …We strongly recommend escalation of therapy.
Conditional Recommendations AGAINST
- For asymptomatic neutropenia and/or lymphopenia (absolute counts <1000/mcL for either) attributed to SLE …We conditionally recommend against initiating immunosuppressive treatment (glucocorticoids, conventional or biologic immunosuppressants) in the absence of other lupus disease activity.
- Cognitive dysfunction: For cognitive dysfunction or decline attributed to active SLE and documented by neuropsychological testing: …We conditionally recommend against addition of immunosuppressive therapy (including glucocorticoid) to cognitive therapy over cognitive therapy alone.
The full manuscript, will be submitted for publication in Arthritis & Rheumatology and Arthritis Care and Research.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.